Macroaneurysm
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Macroaneursym ICD 10 code: H35.09
Disease
Retinal arterial macroaneurysms are acquired, focal dilations of retinal arterial branches (mostly second-order retinal arterioles) that can be classified as hemorrhagic or exudative. Macroaneurysms range from 100 to 250μm in diameter and are most often found in the temporal retina, along the supero-temporal arteriole. Associated findings include capillary telangiectasias, vascular remodeling, and retinal edema. While visual prognosis is generally good, vision loss can occur from macular edema, end-arteriole occlusion from thrombosis, or hemorrhage due to rupture of the aneurysm [1] [2]. Diagnosis is made on clinical exam and via imaging modalities such as fluorescein angiography (FA) and spectral-domain optical coherence tomography (SD-OCT), and treatment is traditionally observation, focal laser photocoagulation, or surgery. More recently, the use of anti-vascular endothelial growth factor (VEGF) intravitreal injections has been suggested but not extensively studied as a possible treatment modality.
Etiology and Pathophysiology
Fichte et al. described vessel wall thickening and the presence of fibrin and foamy macrophages upon histological inspection in retinal arterial macroaneurysms, similar to that seen in age-related arteriosclerotic changes in the vessel walls throughout the body [3]. The localized ischemia due to focal embolic damage to the arterial walls from vascular disease can cause increased intimal collagen remodeling and increased permeability of vessels, thus predisposing the vessel to dilation.
Pathology
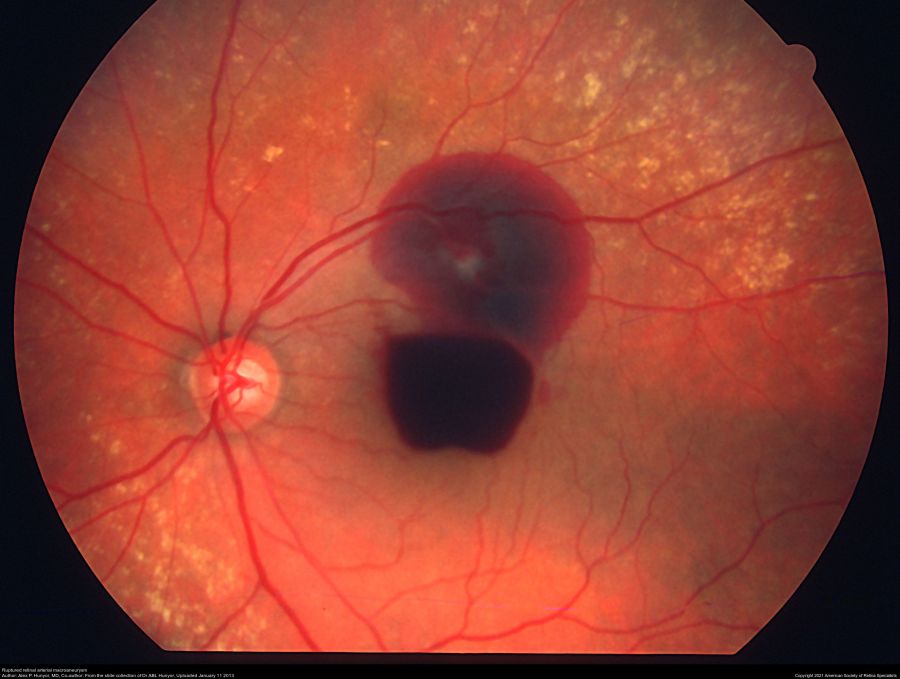
Linear breaks found in arterial walls on histopathology lead to a round or fusiform dilation of the arteriolar vessel wall. This weakened arteriolar wall can rupture and cause hemorrhage and exudation at any level of the retina. If the hemorrhage or exudation affects the macula, the visual acuity is affected.
Epidemiology
The Beijing Eye Study has reported on the incidence of arterial macroaneurysms as being 1 case per 9000 eyes primarily among the adult Chinese population [4]. The majority of those affected are elderly and female [5] [6], and there is a strong association with hypertension (seen in 75% of patients). In hemorrhagic macroaneurysms, 10% of cases are bilateral [2][7] [8].
Primary Prevention
Control of hypertension and arteriolar sclerosis risk factors are the mainstay of prevention.
Diagnosis
Fluorescein angiography can help visualize macroaneurysms which typically fill in the early arterial phase and stain the vessel walls. Possible leakage may be found in later phases.
History
Most commonly, retinal arterial macroaneurysm (RAM) is found incidentally on funduscopic examination in an asymptomatic patient. However, patients may complain of acute vision loss due to macular edema or hemorrhage. Metamorphopsia or decreased vision are most commonly encountered when changes due to macroaneurysms (hemorrhage or edema) affect the fovea. Also presenting complaint may be floaters due to vitreous hemorrhage. Typically, patients have a history of hypertension.
Physical Examination and Imaging
Dilated fundus examination may enable visualization of an out-pocketing of the arterial wall, but in the setting of hemorrhage and/or exudation, it may be necessary to use imaging modalities such as FA and SD-OCT to confirm the diagnosis. Round or fusiform dilation of a retinal arteriole is usually seen within a third degree branch of one of the four main arcade arteries. Most common location for a symptomatic macroaneurysm is from a branch of the superotemporal arcade.
The aneurysm appears as a pulsating round or ovoid pooling of dye on FA, with filling either in the middle to late phase in saccular (sac-like) aneurysms or in the early phase in fusiform (spindle-shaped) aneurysms. SD-OCT can be helpful in quantifying the exudates in the exudative-type macroaneurysm.

Differential Diagnosis
While the presence of a retinal arterial macroaneurysm can be visualized on fundus examination, certain disease processes can present similarly such as Coat’s disease and von Hippel-Lindau disease. Macroaneurysms can also occur secondary to a branch retinal vein occlusion, diabetic retinopathy, radiation retinopathy, and retinal arteritis, in which case the underlying cause should be teased out and treated.
RAM is one of the few causes of hemorrhage at multiple levels (preretinal, retinal, and subretinal hemorrhage). Other causes include anemic/leukemic retinopathy and trauma (shaken baby syndrome).
Management
There are currently no approved guidelines for the management of macroaneurysms. Most macroaneurysms resolve spontaneously. In all patients with this diagnosis, a systematic work-up for hypertension and systemic vascular disease should be pursued.
Complicated retinal arterial macroaneurysms may be directly treated with moderate-intensity laser photocoagulation with two to three rows of large-spot-size (200-500μm) immediately adjacent to the macroaneurysm, especially if visual function is threatened due to increasing edema due to leaking aneurysm [9] [10]. This treatment course is controversial, as some studies have demonstrated a significant decrease in visual acuity in post-laser eyes and possible occurrence of branch retinal arterial occlusion in upto 16% of cases. [11] [12][13].[14].
Cases of submacular hemorrhage can be treated with pneumatic displacement of the clot with or without tissue plasminogen activator, as hemorrhage is toxic to the retina and ellipsoid zone. In cases of premacular hemorrhage, YAG laser can be used to perform a posterior hyaloidotomy and release the hemorrhage into the vitreous for faster clearance.
Recent studies have shown promising results using anti-VEGF agents such as bevacizumab and ranibizumab in patients with macroaneurysm-associated macular edema, with one case series by Pichi et al. demonstrating a reduction in macular edema and hard exudates in all 38 eyes evaluated [15] [16].
Prognosis
The majority of eyes with the diagnosis of arterial macroaneurysm have good visual prognoses and usually regress spontaneously. In general, patients with a hemorrhagic macroaneurysm have a better visual prognosis than those with an exudative macroaneurysm. Patients with persistent macular edema or subretinal hemorrhage have the worst prognosis [2].
Additional Resources
- Porter D, Vemulakonda GA. Blood Pressure. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/anatomy/blood-pressure-list. Accessed January 06, 2023.
References
- ↑ Lee EK, Woo SJ, Ahn J, Park KH. Morphologic characteristics of retinal arterial macroaneurysm and its regression pattern on spectral-domain optical coherence tomography. Retina 2011;31(10):2095-2101.
- ↑ 2.0 2.1 2.2 Moorsavi RA, Fong KC, CHopdar A. Retinal artery macroaneurysms: clinical and fluorescein angiographic features in 34 patients. Eye (Lond) 2006;20(9):1011-1020.
- ↑ Fichte C, Streeten BW, Friedman AH. A histopathologic study of retinal arterial aneurysms. Am J Ophthalmol 1978;85:509-518.
- ↑ Xu L, Wang Y, Jonas JB. Frequency of retinal macroaneurysms in adult Chinese: the Beijing Eye Study. Br J Ophthalmol 2007;91:840-841.
- ↑ Panton RW, Goldberg MF, Farber MD (1990): Retinal arterial macroaneurysms: risk factors and natural history. Br J Ophthalmol 74: 595-600.
- ↑ Rabb MF, Gagliano DA, Teske MP. Retinal arterial macroaneurysms. Surv Ophthalmol 1988;33(2):73-96.
- ↑ Lewis RA, Norton EW, Gass JD (1976): Acquired arterial macroaneurysms of the retina. Br J Ophthalmol 60:21-30.
- ↑ Theodossaidis PG, Emfietzoglou I, Sfikakis PP, Panagiotidis D, Grigoropoulous VG., Theodossiadis GP (2005): simultaneous bilateral visual loss aused by rupture of retinal arterial macroaneurysm in a hypertensive patient. Acta Ophthalmol cand 83:120-122.
- ↑ Bastawrous A, Kumar V, Prasad S. Retinal macroaneurysm following a branch retinal vein occlusion. N Z Med J 2011;124(1344):103-105.
- ↑ American Academy of Ophthalmology. Basic and Clinical Science Course, Section 12, 2011-2012: 173.
- ↑ Ghassemi F, Majidi AR. Development of a second retinal artery macroaneurysm within a few months. Graefes Arch Clin Exp Ophthalmol 2011;249(9):1433-1434.
- ↑ Tsujikawa A, Sakamoto A, Ota M, et al. Retinal structural changes associated with retinal arterial macroaneurysm examined with optical coherence tomography. Retina 2009;29(6):782-792.
- ↑ Brown DM, Sobol WM, Folk JC, Weingeist TA. Retinal arteriolar macroaneurysms: long-term visual outcome. Br J Ophthalmol 1994;78(7):534-538.
- ↑ Xie P, Feng W, Yan R, Zhu S, Gao X. Hemorrhagic retinal arterial macroaneurysm combined with branch retinal artery occlusion treated with intravitreal conbercept injection: A case report. Medicine (Baltimore). 2023 Oct 27;102(43):e35434.
- ↑ Tsakpinis D, Nasr MB, Tranos P, et al. The use of bevacizumab in a multilevel retinal hemorrhage secondary to retinal macroaneurysm: a 39-month follow-up case report. Clin Ophthalmol 5: 1475-1477 (2011)
- ↑ Pichi F, Morara M, Torrazza C, et al. Intravitreal bevacizumab for macular complications from retinal arterial macroaneurysms. Am J Ophthalmol 2013;155(2):287-294.

