Ocular Trauma Score
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Ocular Trauma Score
The Ocular Trauma Score (OTS), proposed by Kuhn et al in the early 2000s, aims to provide a simple system with a few variables to predict the final visual outcome of an injured eye 6 months after open-globe ocular trauma. Over 2,500 eye injuries, across more than 100 variables, were analyzed to develop the OTS.
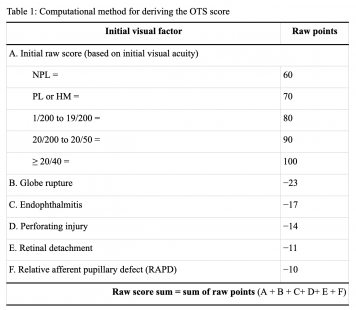
The variables used in the OTS are the initial visual acuity and the presence (or absence) of the following: globe rupture, endophthalmitis, perforating injury, retinal detachment (RD) and afferent pupillary defect (APD).
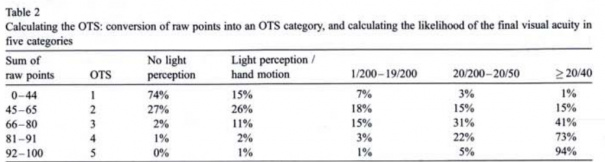
To calculate the raw score, add A + B + C+ D + E + F (Table 1). These raw scores correspond to the OTS (Table 2), which ranges from 1 (more severe injury and worse prognosis) to 5 (less severe injury and better prognosis). The OTS score predicts the probability that visual acuity will fall into various ranges 6 months out from injury.
An adapted version of the OTS, the pediatric OTS (POTS), has been postulated and may be more useful in the pediatric population, as children often struggle to reliably characterize their history of trauma and loss of visual acuity. They also have a tendency for more extensive post-operative inflammation, scarring, and proliferative vitreoretinopathy than adults.6 POTS awards fewer points to the initial visual acuity and considers the patients’ age due to potential resultant amblyopia. However, POTS has been found to significantly underestimate the final visual outcome.6
Significance of the OTS
The OTS is a statistically significant predictor of visual outcomes, and serves as a tool for providers and patients to better understand long-term visual acuity after blunt6 or penetrating7 injuries.
For patients, knowing their OTS can help set realistic expectations for vision potential. The OTS offers prognostic clarity - for patients with a good visual prognosis, it can provide reassurance and assist them in making informed decisions. Additionally, for patients with poor prognosis, the OTS can offer clarity, helping them to prepare emotionally and practically for any difficult decisions ahead (e.g. whether to go forward with elective enucleation).
For the ophthalmologist, the OTS can assist in counseling patients and families, managing expectations of future visual acuity, and providing guidance before pursuing complex interventions. This can improve patient communication and resource utilization. Providers may note that initial visual acuity8,9,10, globe rupture9, retinal detachment8,11, and afferent pupillary defect8,11,12 have been found to be statistically significant variables for poor final visual acuity. Additionally, the OTS can be used for research purposes when evaluating outcomes after ocular injuries.
Limitations of the OTS
It is important to note that the OTS has a 77% probability of predicting the final visual outcome within one visual category.4 While the OTS aids in counseling a patient about their prognosis, its applicability does have some limitations. This arises from the OTS’s tendency to favor extreme predictions, either very poor (Category 1: PL+/HM) or very good vision (Category 2: 20/40 or better), with fewer cases in the moderate categories.6,13 Essentially, the OTS may be less accurate when predicting moderate visual outcomes. Therefore, it should be used as a guideline alongside a comprehensive clinical assessment, rather than a justification for irreversible interventions, such as primary enucleation.
Additionally, while the OTS is an effective prognostic predictor after open-globe trauma, its applicability towards closed-globe injuries remains limited. Closed-globe injuries, such as hyphema, may present with significant initial vision loss but often recover substantially over time. Since the OTS heavily relies on initial acuity, it may underestimate the true visual prognosis of these cases. Although the OTS was originally described for use in both open and closed-globe injuries, its predictive accuracy appears stronger in the open-globe setting. This highlights the need to refine or develop separate scoring systems tailored to closed-globe trauma.
References
1. Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon C (2002) The Ocular Trauma Score (OTS). Ophthalmol Clin North Am 15: 163−166
2. Kuhn F, Maisiak R, Mann L, Morris R, Witherspoon C (2002) The Ocular Trauma Score (OTS): Prognosticating the final vision of the seriously injured eye. In: Kuhn F, Pieramici D (eds) Ocular trauma: principles and practice. Thieme, New York, pp 14−12
3. Weichel ED1, Colyer MH, Ludlow SE, Bower KS, Eiseman AS. Combat ocular trauma visual outcomes during operations iraqi and enduring freedom. Ophthalmology. 2008 Dec;115(12):2235-45. doi: 10.1016/j.ophtha.2008.08.033.
4. Acar U, Tok OY, Acar DE, Burcu A, Ornek F. A new ocular trauma score in pediatric penetrating eye injries. Eye (Lond). 2011 Mar;25(3):370-4. doi: 10.1038/eye.2010.211.
5. Scott R. The Ocular Trauma Score. Community Eye Health. 2015;28(91):44-45.
6. Chaudhary A, Singh R, Singh SP. Prognostic value of Ocular Trauma Score and pediatric Penetrating Ocular Trauma Score in predicting the visual prognosis following ocular injury. Rom J Ophthalmol. 2022;66(2):146-152. doi:10.22336/rjo.2022.29
7. Yaşa D, Erdem ZG, Demircan A, Demir G, Alkın Z. Prognostic value of ocular trauma score for open globe injuries associated with metallic intraocular foreign bodies. BMC Ophthalmol. 2018;18(1):194. Published 2018 Aug 9. doi:10.1186/s12886-018-0874-3
8. Deud BG, Hammerschmidt HF, Kniggendorf MV, Hopker LM, Müller GG. Ocular trauma score as a visual prognostic factor of open globe injuries in a hospital of southern Brazil. Arq Bras Oftalmol. 2021;84(6):576-581. doi:10.5935/0004-2749.20210095
9. Ho H, Foo J, Li YC, et al. Prognostic factors and epidemiology of adult open globe injuries from Western Sydney: a twelve-year review. BMC Ophthalmol. 2021;21(1):173. Published 2021 Apr 10. doi:10.1186/s12886-021-01929-z
10. Yu Wai Man C, Steel D. Visual outcome after open globe injury: a comparison of two prognostic models--the Ocular Trauma Score and the Classification and Regression Tree. Eye (Lond). 2010;24(1):84-89. doi:10.1038/eye.2009.16
11. Meng Y, Yan H. Prognostic Factors for Open Globe Injuries and Correlation of Ocular Trauma Score in Tianjin, China. J Ophthalmol. 2015;2015:345764. doi:10.1155/2015/345764
12. Rofail M, Lee GA, O’Rourke P. Prognostic indicators for open globe injury. Clin Exp Ophthalmol. 2006;34(8):783–786. doi: 10.1111/j.1442-9071.2006.01309.x.
13. Watanachai N, Choovuthayakorn J, Nanegrungsunk O, et al. Intraocular foreign body: Characteristics, visual outcomes, and predictive values of ocular trauma score. Heliyon. 2023;9(10):e20640. Published 2023 Oct 4. doi:10.1016/j.heliyon.2023.e20640