All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Monocular elevation deficit or double elevator palsy
Disease
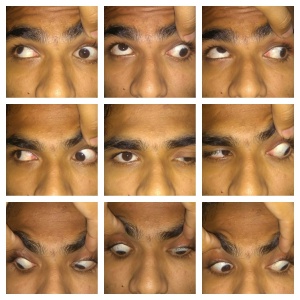
Monocular Elevation Deficiency (MED) is the limitation of elevation of the affected eye that is similar in both adduction and abduction. MED is one of the causes of hypotropia and can be associated with ptosis/pseudoptosis.
Etiology
MED can be congenital or acquired.
- Congenital cases of MED occur sporadically.[1] The causes include supranuclear palsy, primary superior rectus paresis and primary inferior rectus restriction.[2]
- Acquired cases are usually caused by trauma, cerebrovascular diseases like hypertension, thromboembolism, sarcoidosis and syphilis or tumors such as pineocytomas, acoustic neuromas and metastases.[3]
General Pathology
There are generally thought to be three forms of this motility disorder: inferior rectus restriction; deficient innervation of the elevator muscles; or a combination of restriction and elevator deficit. [4]
- In Type 1, the etiology is inferior rectus restriction, such as primary inferior rectus restriction or fibrosis. Forced duction test (FDT) demonstrates a tight inferior rectus. The upward saccades are usually normal until the tight inferior rectus limits upgaze. Bell's phenomenon is usually poor.
- In Type 2, the etiology is deficient innervation of the elevator muscles, and includes primary superior rectus palsy. FDT is free and upward saccades are slow both below and above midline. Bell’s phenomenon is usually absent.
- In Type 3, the etiology is the supranuclear type and is usually congenital. It is characterized by intact or mildly reduced vertical saccadic velocity below midline but abnormal or absent velocity above midline. FDT is unlimited.
Pathophysiology
Efferent tracts for upgaze leave the rostral interstitial nucleus of the medial longitudinal fasciculus, cross the midline in the posterior commissure, course through the pretectum and enter the superior rectus subnucleus of the oculomotor nucleus, leave the subnucleus, and cross the midline again. As a result of double decussation, the superior rectus receives innervation from ipsilateral rostral interstitial nucleus of the medial longitudinal fasciculus as well as contralateral pretectum and superior rectus subnucleus. In cases of MED, it is presumed that supranuclear input from the rostral interstitial nucleus of the medial longitudinal fasciculus into third cranial nerve nucleus is interrupted. Supranuclear deficiency affects upgaze, therefore causing deficient elevation.
Diagnosis
Chief Complaints
Patients can present with the following complaints:
- Vertical misalignment of the eyes
- Diplopia
- Abnormal head posture
- Inability to elevate the affected eye
- Drooping of eyelid
- Decreased vision
Signs
- Ptosis/Pseudoptosis: Ptosis can be associated with hypotropia because of fascial attachments between the levator palpebrae superioris and superior rectus muscle. Pseudoptosis can be present in primary gaze when fixating with the contralateral eye, however improves when the hypotropic eye takes up fixation. Both pseudoptosis and true ptosis can be present in the patient.
- Strabismus: There is hypotropia of the affected eye when the unaffected eye is fixing and hypertropia of the contralateral eye when fixating with the affected eye.
- Bell’s phenomenon: The phenomenon is typically absent in cases of inferior rectus restriction and superior rectus palsy, but is usually present in cases of MED resulting from supranuclear defects.
- Amblyopia: Asymmetric vision may be present if there is a constant deviation of affected eye, ptosis, or anisometropia.
- Abnormal Head Posture : Most commonly the patient has a chin elevation if binocular fusion is present. Abnormal head posture may not be present if the affected eye is amblyopic.
- Saccades: Upward saccades are slow in cases of superior rectus palsy, absent above the midline in supranuclear palsy, and intact but stop abruptly in cases associated with inferior rectus restriction.
Diagnostic Procedures
Forced Duction Test
Forced duction test is a clinical test to evaluate for restriction. The test is performed under topical or general anesthesia. The conjunctiva is held at limbus with forceps and the globe is rotated by the examiner.
Active Force Generation Test
Active force generation test is done under topical anesthesia by asking the patient to look in the direction of the muscle being tested.
Worth Four Dot
Worth Four Dot testing is done with red and green glasses (red over the right eye) to dissociate the images from each eye. The test is performed at distance and near.
Differential diagnosis
The main differential diagnosis of MED includes:
- Brown syndrome - characterized by limitation of elevation in adduction with Y pattern exotropia
- Duane syndrome - diagnosed by the presence of globe retraction in downgaze along with limitation of elevation in upgaze
- Congenital fibrosis of the extra ocular muscles -may initially affect the inferior rectus muscles and thus be misdiagnosed as MED. Bilateral presentation and involvement of other extraocular muscles help distinguish it.
- Partial third nerve palsy - particularly if involving the superior division of oculomotor nerve
- Progressive external ophthalmoplegia - differentiated as it involves multiple extraocular muscles
- Orbital inflammatory disease
- Orbital cellulitis
Management
Management of MED includes both non-surgical and surgical components.
Non-Surgical Management
It is important to correct any underlying refractive error and treat amblyopia.
Surgery
The goal of surgery is to improve the position of the affected eye in primary gaze and to increase binocular field of vision.
Indications for surgery include:
- Significant vertical deviation in primary gaze
- Significant abnormal head posture
- Deviation-induced amblyopia
- Diplopia in primary gaze
- Restricted binocular fields
In general, the surgery of choice in the management of MED depends on results of the forced duction test. In patients with a positive forced duction test, inferior rectus recession is the first choice of management. If there is no restriction, transposition of the medial and lateral rectus muscles to the superior rectus muscle can be performed (Knapp procedure). Other options include resection of the ipsilateral superior rectus muscle or recession of the contralateral superior rectus muscle.
In greater detail:
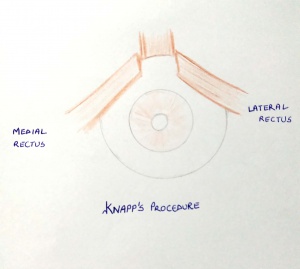
- Knapp's procedure [5]
The medial and lateral rectus muscles are transposed to the insertion of the superior rectus muscle. In Knapp’s own study, the procedure showed marked variability correcting 21-55 PD (average 38 PD) hypotropia.
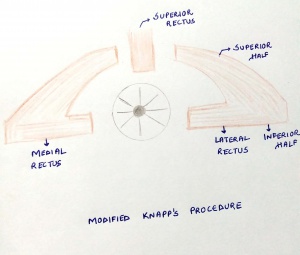
- Modifications of Knapp's procedure[6]
For cases with an associated horizontal deviation, a partial tendon Knapp’s procedure has been described. In this procedure, the superior halves of the equally divided horizontal muscles are placed near the superior rectus muscle insertion, which allows for correction of the horizontal deviation with the inferior halves.
- Augmented Knapp's procedure
Augmented Knapp's procedure utilizes Knapp's procedure combined with posterior fixation sutures on the horizontal recti to increase its effect.
- Modified Nishida's for monocular elevation deficit[7]
A technique by Nishida et al that was originally described for abducen nerve palsies can be used to correct up to 30 PD of vertical deviation with low risk of anterior segment ischemia.
- Contralateral superior rectus recession [8]
Contralateral superior rectus recession may be an option in patients with residual hypotropia after inferior rectus recession.
Ptosis can be addressed after the vertical deviation has been corrected to ensure the pseudoptosis element has been eliminated.
Management of Acquired MED
As there are wide variety of causes of acquired MED, a thorough workup should be performed. The management varies according to the underlying cause.
Complications
Surgical complications that may occur when treating MED include:
- Overcorrection and undercorrection
- Tenon's prolapse
- Conjunctival cyst
- Corneal dellen formation
- Anterior segment ischemia
Additional Resources
- Porter D, Vemulakonda GA. Blood Pressure. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/anatomy/blood-pressure-list. Accessed January 06, 2023.
References
- ↑ Bagheri A, Sahebghalam R and Abrishami M. Double Elevator Palsy, Subtypes and Outcomes of Surgery. Journal of Ophthalmic & Vision Research 3.2 (2008): 108.
- ↑ Jampel RS, Fell P: Monocular elevation paresis caused by a central nervous system lesion. Arch Ophthalmol 1968: 80:4.
- ↑ Rosenbaum AL. Clinical strabismus management. 1st ed. Philadelphia: WB Saunders; 1999.
- ↑ Ziffer AJ, Rosenbaum AL, Demer JL, Yee RD. Congenital double elevator palsy: vertical saccadic velocity utilizing the scleral search coil technique. J Pediatr Ophthalmol Strabismus. 1992; 29:142–9.
- ↑ Knapp P. The surgical treatment of double elevator paralysis. Trans Am Ophthalmol Soc. 1969; 67:304–23
- ↑ Kamlesh, Dadeya S. Surgical management of unilateral elevator deficiency associated with horizontal deviation using a modified Knapp’s procedure. Ophthalmic Surg Lasers Imaging. 2003; 34:230–5.
- ↑ Sowmya Ravendra Murthy, Mithuna Pappuru,Modified Nishida's procedure for monocular elevation deficiency JAAPOS, 2018 August;327-329
- ↑ Ocak OB, InalA et al Surgical Management in Type 1 Monocular Elevation Deficiency J Pediatr Ophthalmol Strabismus. 2018 Nov 19;55(6):369-374.
- Kocak-Altinas AG et al Binocul Vis Strabismus Q. 2000; 15:39–46.
- Burke JP, Ruben JB, Scott WE. Br J Ophthalmol. 1992; 76:734–7.
- Caldeira JA. Vertical transposition of the horizontal rectus muscles for congenital/early onset ″acquired″ double elevator palsy: A retrospective long term study of 10 consecutive patients. Binocul Vis Strabismus Q. 2000;15:29–38.
- Snir M, Friling R, Kalish-Stiebel H et al. Ophthalmology. 2005;112:933–8.