All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Vertical strabismus refers to the misalignment of the visual axes in the vertical direction such that one eye is higher than the other. The prevalence of vertical deviations associated with horizontal strabismus or as isolated entities is high. Scobee at al[1] noted a vertical component in 43% of patients with esotropia. As the 4 principal muscles involved in vertical ductions also cause an element of cyclotorsion, it is impossible to separate them from each other. Thus, the term ‘cyclovertical’ strabismus is better suited for such deviations. It is important to distinguish these from horizontal deviations for several reasons:
- Sensory adaptations (amblyopia/anomalous retinal correspondence) are noted much less frequently.
- Comitance is rare.
- The magnitude of deviations is smaller.
- Due to low vertical fusional reserve (3-5 Δ[2]), a small vertical deviation can cause diplopia or blurring of vision.
Terminology
The deviation is denoted based on the direction of the non-fixating eye. In case of alternating deviations, by convention we designate the vertical squint by the upwards deviating eye. If the deviation is similar in all 9 gazes, the deviation is said to be comitant whereas if the deviation varies in different gazes, it is said to be incomitant.
Phorias refer to a latent deviation which is compensated for by the fusional amplitude reserve whereas Tropias refer to a manifest deviation that has exceeded the fusional capacity and leads to a disruption of binocular single vision.
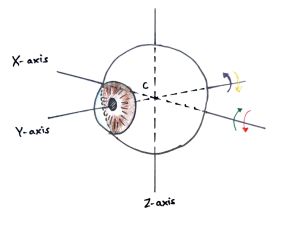
Hyperdeviation: the visual axis is rotated along horizontal axis (X-axis) such that cornea is displaced superiorly and fovea inferiorly. (Figure 1, green arrow)
Hypodeviation: the visual axis is rotated along horizontal axis (X-axis) such that cornea is displaced inferiorly and fovea superiorly. (Figure 1, red arrow)
Incycloduction (intorsion): the eye is rotated along an antero-posterior axis (Y axis) such that the superior limbus is tilted nasally. (Figure 1, orange arrow)
Excycloduction (extorsion): the eye is rotated along an antero-posterior axis (Y-axis) such that the superior limbus is tilted temporally. (Figure 1, purple arrow)
Pseudovertical strabismus: the appearance of a vertical deviation when the visual axes are actually aligned and binocular single vision maintained such as in cases of orbital asymmetry, eyelid retraction, ptosis, globe displacement due to an orbital mass lesion, vertical angle kappa, facio-maxillary fractures etc.
Applied Anatomy and Physiology
The 4 principal muscles involved in vertical movements of the eyeball and their primary, secondary, and tertiary actions are as follows (Table 1):
| Muscle | Nerve Supply | Primary Action | Secondary Action | Tertiary Action |
|---|---|---|---|---|
| Superior Rectus | Superior division of oculomotor nerve (CN III) | Elevation | Intorsion | Adduction |
| Inferior Rectus | Inferior division of oculomotor nerve (CN III) | Depression | Extorsion | Adduction |
| Superior Oblique | Trochlear nerve (CN IV) | Intorsion | Depression | Abduction |
| Inferior Oblique | Inferior division of oculomotor nerve (CN III) | Extorsion | Elevation | Abduction |
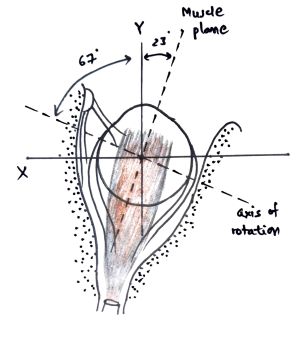
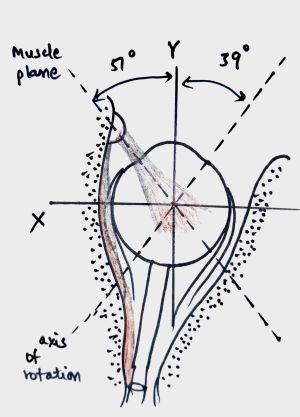
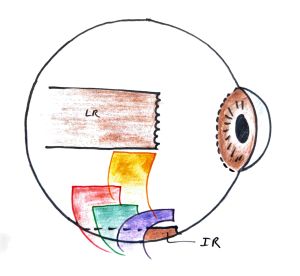
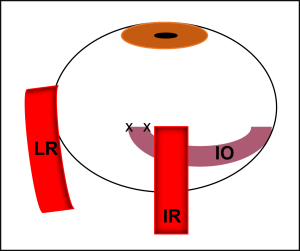
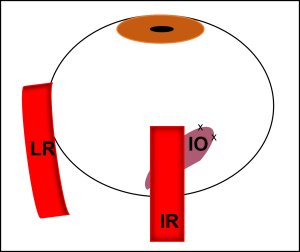
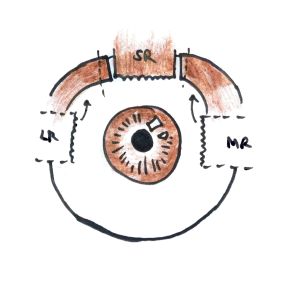
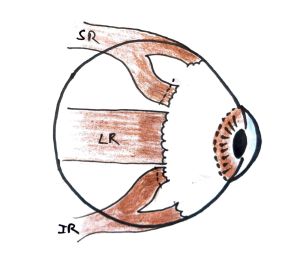
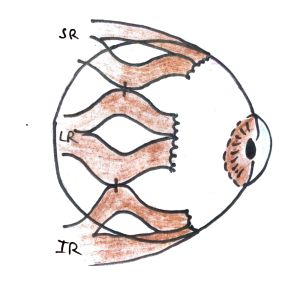
These can be better understood by the following illustrations (Figure 2 and 3).
The muscles causing torsional movement in an eye have opposing vertical actions that balance each other out. For example, the intorters SO and SR have opposing vertical actions (depression and elevation respectively) such that there is no net vertical movement during intorsion and vice versa. This forms the basis of the Park-Bielschowsky three step test (See below).
For coordinated vertical movements, the vertical rectus muscle of one eye yokes with the oblique muscle of the other eye and vice versa. For example, the right superior rectus and left inferior oblique are yoke muscles for dextro-elevation and receive equal innervation according to Hering’s law.
Etiology
The various etiologies of cyclovertical deviations are as follows:
- Comitant Hyperdeviation
- Incomitant Hyperdeviation
- Neurogenic palsy
- Supranuclear (gaze) palsy
- Nuclear
- Infranuclear palsy
- cranial nerve III/IV palsies
- Myogenic dystrophies and Myasthenia gravis
- Anatomical restrictions
- Vertical Duane Retraction Syndrome
- Brown’s syndrome
- Congenital Fibrosis of Extraocular Muscles
- Monocular elevation deficit syndrome
- Craniosynostosis
- Heavy eye syndrome
- Sagging eye syndrome
- Thyroid ophthalmopathy
- Orbital wall fractures
- Tumors, pseudotumors and other orbital mass lesions
- Anti-elevation syndrome after Inferior oblique anteriorization (iatrogenic strabismus)
- Deviations with primary overaction of Inferior oblique
- Neurogenic palsy
- Dissociated Vertical Deviation (DVD)
- Cyclovertical motility abnormalities with horizontal deviations: AV pattern strabismus
Preoperative Evaluation
History
A detailed history with special emphasis on age of onset, percentage of time eye(s) deviated, misalignment present with distance viewing and/or near viewing, anomalous head positions, family history, medications, health problems, history of trauma and previous treatments should be undertaken.
Symptoms
A patient with cyclovertical deviation can present with the following complaints:
- Double vision or diplopia
- Cosmetically unacceptable vertical deviation
- Anomalous head posture
- Asthenopic symptoms such as headache, blurring of vision etc.
Clinical Examination
A thorough general ophthalmic examination must include visual acuity with current correction, best corrected visual acuity, stereoacuity, ocular motility, slit lamp examination, a dilated fundus examination using indirect ophthalmoscope to determine ocular torsion and cycloplegic refraction.
Anomalous Head Posture
A detailed evaluation of head posture is of the utmost importance, especially in deviations of paretic origin. The patients habitually hold their heads in a position in which they can avoid the field of action of the paretic muscle to avoid diplopia and to maintain binocular single vision. The type of head posture is noted: face turn, head tilt and/or chin elevation or depression. Old family photographs, if available, can be used to corroborate the duration of the head posture.
Ocular Deviation
The magnitude of misalignment of the eyes should be checked in all 9 gazes and head tilt right and left and can be done by objective as well as subjective means.
Objective tests: These tests do not rely on the patient’s response.
- Corneal reflex tests (Hirschberg, Krimsky)
- Cover-uncover tests using prism bars or synoptophore
- Fundus imaging
- Ophthalmoscopy
Subjective tests: These tests rely on the patient’s cooperation and response. These tests are considered a better indicator of the patient's sensory system.
- Synoptophore
- Diplopia charting
- Hess charting
- Double Maddox rods
- Worth 4-dot test
- Bagolini striated glasses
- Blind spot charting on perimetry
Ocular Motility
It is important to note the limitations of movements (ductions and versions) in all 9 gazes. In restrictive squints the limitation of movements is much greater compared to the angle of deviation whereas in paretic squints these two corroborate each other.
The overaction or underaction of the muscles can be subjectively graded on 7-point (+3 to -3) or 9-point (+4 to -4) scale. An indirect method to document oblique overaction is to assess the pupillary position with respect to the lid margin on adduction.[3] The severity of IOOA was graded from 0 to +4 as follows: (0) no IOOA, (+1) mild upwards deviation of the pupil from the horizontal line in adduction, (+2) upper margin of the pupil becomes aligned to the margin of the upper lid in adduction, (+3) superior half of the pupil covered by the upper lid in adduction, and (+4) the entire pupil covered by the upper lid in adduction.
FDT and Exaggerated FDT
Forced duction test (FDT) was first described to evaluate Duane syndrome in the 1900s.[4] It is critical for determining the etiology of an underacting recti muscle: restrictive or paretic and for formulating the surgical plan. It can be performed as an office procedure as well as intraoperatively. The other eye is patched and after instillation of a topical anesthetic solution in the eye to be examined, the conjunctiva is grasped at the limbus using a non-traumatic forceps taking care not to push the globe into the orbit which can lead to false positive results.[5] The eye is then rotated passively in the direction opposite that in which mechanical restriction is suspected. For instance, to distinguish between LR paresis and MR restriction, the eye is passively rotated into full abduction. If the movement is full and free, the defect is clearly due to LR paralysis.
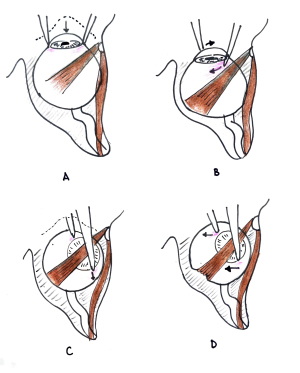
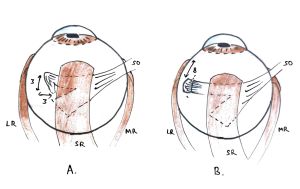
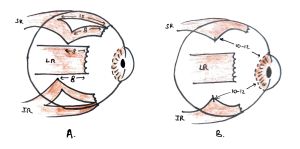
Exaggerated forced duction test was devised by Guyton to evaluate tightness of the oblique muscles.[6] In contrast to conventional FDT, the globe is retroplaced into the orbit to exaggerate the restriction of the obliques (Figure 4A). For superior oblique, the globe is held firmly at 9 O’clock and 3 O’clock limbal position. The globe is then extorted while maintaining retroplacement and pushed superonasally (Figure 4B and 4C). Both the forceps are then moved temporally with the temporal forceps almost in line with the nasal forceps (Figure 4D). A normal or taut oblique muscle would cause the globe to ‘jump’ or ‘pop out’ as the tendon slips nasally over the globe surface to a less stressed position. A lax or weakened muscle would not show this response. After a weakening procedure, a positive test indicates insufficient weakening.
Parks Bielschowsky 3-Step Test
This test is applicable in paresis of any of the 4 cyclovertical muscles. However, the diagnostic accuracy is higher for oblique paresis as the vertical action of recti muscle are much more than the vertical action of obliques. This test must be done in supine posture due to the orientation of the semicircular canals. The simplicity and ingenuity of this test can be understood by examining a case of right hyperdeviation (figure 5):
Step 1: Right or Left hypertropia in primary gaze?
In case of right hypertropia, either the depressors of right eye (RIR and RSO) or elevators of left eye (LSR or LIO) are paralyzed.
Step 2: Deviation increasing on dextroversion or levoversion?
Muscles with greater vertical action in that direction are underacting.
- Elevation increases on dextroversion: LIO in adduction and RIR in abduction
- Elevation increases on levoversion: RSO in adduction and LSR in abduction
Step 3: (Bielschowsky Head tilt test): Deviation increasing on head tilt?
Muscles with compensatory action are underacting.
- Elevation increases on right head tilt: right intorters- RSO and RSR and left extorters- LIR and LIO
- Elevation increases on left head tilt: left intorters- LSO and LSR, and right extorters- RIR and RIO.
The muscle common to all the 3 steps is identified as the underacting muscle.
Limitations
Though simple in its application, there are several fallacies to this test:
- Restrictive strabismus
- Paresis or more than one EOM
- Previous surgical manipulation of EOMs
- Myasthenia gravis
- Skew deviation
- Dissociated vertical deviation
Diplopia Charting
Used in conjunction with red-green dissociation, a horizontal light source is used in cases of cyclovertical deviations. This leads to maximum separation of images vertically and allows for observation of tilt. In case of DVD, a red filter alone is used. The red image is perceived lower irrespective of the filter being over either eye because it is always the eye behind the filter which manifests upward deviation.
Non-Surgical Management
There is a limited role of non-surgical management in cyclovertical deviations. This can be attributed to a small vertical fusional reserve which leads to symptoms of diplopia or confusion even in cases with small deviations. Additionally, there is a paucity of association with sensory adaptations (suppression, amblyopia or ARC) and accommodation anomalies and thus various treatment modalities such as orthoptics, convergence exercises have not found widespread use for cyclovertical deviations. However, the patient must undergo cycloplegic refraction and any refractive error or associated vergence anomaly must be properly addressed. Small vertical deviations can be managed by prisms, especially residual or consecutive deviations.
Chemodenervation
Botulinum toxin A (BTA) intramuscular injections have been used as an alternative or adjunct to muscle weakening procedures. The majority of existing literature deals with its application in childhood/infantile horizontal tropias[7][8][9] and paretic horizontal strabismus particularly abducens nerve palsy.[10][11] Chemodenervation in vertical squint is being explored and the following indications have been documented.
- While performing full vertical rectus transposition (VRT), injection of botulinum toxin into the medial rectus is an alternative to medial rectus recession which increases the risk of anterior segment ischemia.[7]
- In thyroid-associated orbitopathy (TAO), BTA has been shown to improve motility, reduce diplopia, and decrease surgical dose in subsequent operations.[12]
- In traumatic superior oblique (SO) palsy, BTA injection into the ipsilateral antagonist (IO) may be a useful adjunct for reducing symptomatic diplopia.[13]
- Inferior rectus BTA injections for iatrogenic vertical strabismus[14] and inflammatory conditions.[15]
Cyclovertical Strabismus Surgery
Inferior Oblique
Inferior oblique is a unique EOM in being the only muscle that does not originate from the orbital apex. It arises from the orbital surface of the maxilla and inserts on the posterior inferolateral aspect of the eyeball under the lateral rectus muscle.[16] It is innervated by the inferior division of the oculomotor nerve (IIIrd nerve) and the blood supply is by the infraorbital artery. It is an elevator, abductor, and extorter.[17] Other than being the smallest muscle (36-37mm) and having the shortest tendon (2mm), it is also the only muscle to come in contact with 2 other muscles: IR and LR.
Inferior oblique overaction (IOOA) manifests as overelevation in adduction and is usually associated with horizontal deviations. The cause can be primary or secondary. Primary IOOA is most commonly associated with infantile esotropia, accommodative esotropia, and intermittent exotropia and the etiology remains unknown.[18] Secondary reasons include superior oblique palsy. Surgical methods to weaken the inferior oblique include myectomy, myotomy, tenectomy, recession, anterior transposition, antero-nasal transposition, denervation-extirpation, and disinsertion. However, recession has been shown to be the most effective procedure that prevents return of IOOA.[19][20] Recessions will lead to weakening of the primary action of IO i.e. extorsion whereas anteropositioning will have the added effect of weakening elevation also.
Inferior oblique underaction is seen in Brown’s syndrome and inferior oblique palsy.[21] Strengthening procedures on IO are limited. Due to a very small tendinous portion, resection procedures are not applicable. In case of IO palsy, recession of contralateral yoke muscle (SR) or weakening of ipsilateral antagonist (SO) can be done. Vertical prisms can be employed to manage small amounts of vertical deviations.
Indications for IO Weakening Procedures
- Primary inferior oblique overaction
- Dissociated vertical deviation
- V-pattern with IOOA
- Superior oblique palsy
- Excyclotorsion
- Torsional Kestenbaum procedure
- Monocular Elevation Disorder (contralateral inferior oblique)
- Duanes Retraction syndrome with IOOA
Contraindications for IO Weakening Procedures
- V-pattern strabismus without IOOA
- X-pattern strabismus
- Craniofacial syndromes with apparent IOOA
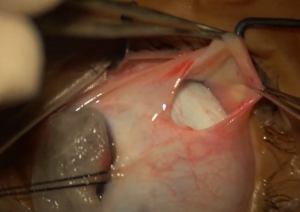
Isolating the Muscle
- Inferotemporal limbus is grasped by the assistant and the globe rotated in elevation and adduction
- Conjunctival incision is made in the inferotemporal quadrant 8mm from the limbus[22]
- Intermuscular septum and tenon’s fascia is dissected to expose bare sclera
- LR muscle is secured with a muscle hook
- After careful dissection of its fascial attachments and periorbital fat, IO is hooked taking extra care not to injure the inferotemporal vortex vein
- Adhesions between the insertion of the IO and the sclera are severed to expose whole width of IO insertion
Surgical Techniques
Recession
After isolation of the inferior oblique muscle there are a variety of approaches to muscle imbrication:
- 6-0 absorbable suture is passed through the entire width of the tendon 1mm from insertion and locking knots placed on both sides. The IO is finally disinserted using Westcott scissors
- The muscle is disinserted close to the insertion and 6-0 polyglactin sutures are passed just posterior to the clamp.
The disinserted muscle can be reinserted at several advocated points for different amounts of recession as follows:
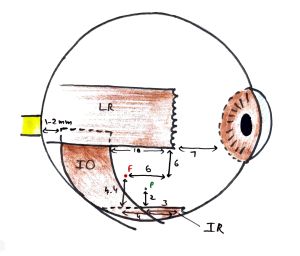
Fink's Point/Fink's Recession Technique[23]
In his original approach, using the lateral rectus as a landmark, Fink reinserted the anterior edge of IO 6mm inferior and 6mm posterior from the anterior end of the inferior edge of LR insertion (Figure 6). The posterior end was reinserted 6mm posterior to the recessed anterior end parallel to the lateral border of IR. This provides a total recession of 8mm (Figure 7, Red). To avoid unnecessary exposure of LR, the Fink’s point can also be located by using IR as a landmark (4mm posterior and 4.4mm superior to the lateral border of IR).[24]
For an 8 mm recession, the anterior point is 6 mm inferior and 6 mm posterior to the inferior edge of the lateral rectus insertion and the posterior point is 5-6 mm posterior to the anterior point. For a 10 mm recession, the IO is inserted 8mm posterior and 2 mm inferior to the lateral rectus insertion
Scheie-Park Point/Park's Recession Technique[19][20]
Initially used by Scheie and popularized by Park, this method reinserts the anterior end of IO 3mm posterior and 2mm superior to the lateral border of IR (Figure 6). The posterior end is reinserted 5-6mm laterally and 1mm behind the anterior tip. Though initially advocated as an 8mm recession by Park, further studies have shown that this method leads to 10.4mm recession and around 1mm anteropositioning (Figure 7, Green).[24] Probably this is the reason that it has been found to have a stronger weakening effect compared to larger recessions of 12-14mm.[25]
Elliott and Nankin's Recession Technique
The anterior end of IO is inserted at the lateral end of the inferior rectus insertion and the posterior end is 5 mm posterior.
Graded Recessions[24][26]
Advocating lateral border of IR to be used as a landmark for IO recessions, several points for reinsertion along the course of IO have been shown to lead to graded recessions. Taking Fink’s point as 8mm recession site, any relocation upwards or downwards along the course will lead to less or more recession respectively (Table 2).
| Desired Recession (mm) | Measured posteriorly from IR insertion (mm) | Measured superiorly from lateral border of IR (mm) |
|---|---|---|
| 6 | 5.0 | 6.4 |
| 7 | 5.0 | 5.4 |
| 8 | 4.0 | 4.4 |
| 9 | 4.0 | 3.4 |
| 10 | 4.0 | 2.4 |
| 11 | 4.0 | 1.4 |
| 12 | 4.0 | 0.4 |
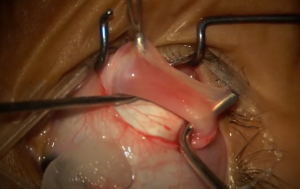
Anterior Transposition
Anterior transposition has been shown to work in part by converting the IO from an elevator to a depressor of the globe as the neurovascular bundle becomes a new origin for the temporal portion of the IO.[27] Introduced by Gobin,[28] this method has been shown to be extremely useful in DVD, primary IOOA and secondary overaction due to SO palsy.[29] The anterior fibers of the isolated IO muscle are reinserted temporal to IR insertion and the posterior fibers are bunched up with the anterior fibers (Figure 7, Blue). If the new insertion site is fanned out, there is an increased likelihood of restriction of elevation which has been labelled as ‘Anti-Elevation Syndrome’ (AES).[30] Anteriorization can also be graded by using the IR insertion site as ‘zero’ station, 1mm anteriorly as ‘+1’ and 1mm posteriorly as ‘-1’ and so forth.
Pure/Total Anteropositioning[31]
The disinserted ends of IO are simply reinserted anteriorly adjacent to the inferior edge of LR insertion (Figure 7, Orange). This produces anteropositioning without any recession. Thus, it does not change the torsional status. It has been found to be comparable to Fink’s 8mm recession and useful in mild to moderate IOOA or dissociated vertical deviation with IOOA.[32]
Anterior and Nasal Transposition[33]
In Anterior and Nasal Transposition (ANT) of the IO muscle, the new insertion is 2 mm nasal and 2 mm posterior to the nasal border of the IR muscle insertion. ANT converts the IO muscle into an intorter and depressor and improves elevation in adduction. This procedure is useful in patients with severe or recurrent congenital and acquired superior oblique palsies, especially when performing a secondary procedure.
Nasal Myectomy[34]
Nasal myectomy is found to be effective in cases with residual IOOA even after anteriorization has been performed. The IO is hooked at the anteriorized end and dissected along its course to the nasal end. Two muscle clamps are placed 5 mm apart. The muscle tissue is resected between the clamps, ends are cauterized before being released. The temporal portion of the IO then acts as the new origin of the muscle since the neurovascular bundle is present here.
Myotomy
Myotomy is a self-adjusting procedure in which the muscle is incised close to the insertion and allowed to retract without placing any sutures. The result of this procedure is unpredictable since if the muscle has more overaction then it may contract more as compared to a muscle that has less overaction.[35]
Myectomy
This is also a self-adjusting procedure in which 2 clamps are placed, one close to the insertion and the other 4 to 8 mm from the first clamp.[21] The muscle is excised between the clamps and the ends are cauterized to prevent bleeding. Reoperations may be difficult as it is not easy to relocate the muscle.
A recent meta-analysis has found IO myectomy comparable to IO anteropositioning in the management of IOOA as they produced comparable outcomes in the improvement in hypertropia, post-operative inferior oblique function and incidence of complications.[36] Nasal myectomy has been shown to be an effective supplementary procedure for the correction of residual IOOA following anteropositioning.[34][37]
Denervation and Extirpation
This procedure involves cauterization of the neurovascular bundle combined with a large myectomy for severe IOOA.[38] This extreme procedure precludes any further procedure on IO in case of residual overaction and due to the success of large recessions and anteropositioning for severe IOOA, it has become largely obsolete. Based on the degree of hypertropia in upgaze (for unilateral IOOA) and degree of overaction (for bilateral IOOA), the recommended IO weakening procedures (in increasing order of weakening) are: 12-14mm recession, 10mm recession and anteropositioning.[39]
Inferior Oblique Muscle Weakening Procedures Video
Surgical Complications
Complications can occur following inferior oblique recession. These include undercorrection, overcorrection, hemorrhage, pupil dilation and fat adherence syndrome.[40]
Hemorrhage
Since the IO is a highly vascularized muscle, it can bleed profusely during surgery. Blood can go subconjunctival and even beneath the eyelid to cause ecchymosis. Optic atrophy can occur if hemorrhage occurs near the optic nerve region. Perforation of the vortex vein can also lead to bleeding.
Pupil Dilation
Excessive trauma to the IO can cause pupillary dilation as a result of damage to the nerve to the ciliary ganglion that bears the parasympathetic fibers to the pupil. Mydriasis can be temporary or permanent. Permanent mydriasis may also be a result of hemorrhage in the optic nerve region.
Fat Adherence Syndrome
Rupture of the posterior tenon’s can lead to prolapse of adipose tissue in the inferotemporal quadrant.
Superior Oblique
The longest EOM, SO has a fan shaped tendinous insertion beneath the SR. The posterior fibers of the fan are majorly responsible for depression and the anterior fibers responsible for intorsion. It is supplied by the trochlear nerve (cranial nerve IV).
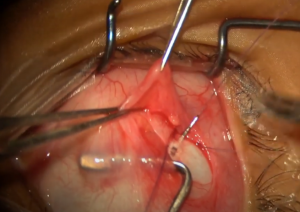
Isolating the Muscle
- The conjunctiva is incised 8mm from limbus in the superotemporal quadrant
- Incision is enlarged 6mm circumferentially in nasal direction
- SR muscle is hooked and used to rotate the globe inferiorly
- Muscle hook is used to push the nasal extent of the incision to aid in visualization of intermuscular septum nasal to SR
- SO tendon is identified near the nasal border of SR
- A buttonhole incision is made in the intermuscular septum to expose whole width of the tendon
- SO tendon is isolated on a small muscle hook
SO Strengthening Procedures
The major indication for SO strengthening procedures is cranial nerve IV palsy.
SO Tuck or Tenoplication
This is the preferred surgery for generalized strengthening of SO and is particularly favored in patients with severe SO underaction with minimal IOOA. The great advantages of the tucking operation on the superior oblique are (1) it practically always straightens the head, (2) it greatly reduces the hyperdeviation, and (3) it has no effect on the width of the lid fissures.[41] It corrects torsion in the primary position and up to 12 degrees in downgaze, while also correcting as much as 15 Δ of vertical deviation.
Exaggerated FDT is done at the beginning of the procedure to assess laxity of the tendon. After the tendon is isolated and hooked as described above, it is lifted to double fold over itself and a resection clamp applied. The tuck is performed temporal to the SR by imbricating the anterior and posterior halves of the folded over tendon using interrupted 6-0 absorbable sutures. Exaggerated FDT is repeated to assess the adequacy of the tuck. The inferior limbus should reach the horizontal meridian during passive elevation in adduction.[42]
Iatrogenic Brown syndrome is the most common complication encountered after SO tuck.[43] It can be prevented by forced duction testing of the SO during surgery. Excessive restriction or intolerable diplopia should be addressed in the immediate post-op period by releasing or reducing the amount of SO tuck.
Anterior fiber tuck has been described as a modification to treat symptomatic excyclotorsion without vertical deviation.[44][45] The tendon is split between the anterior one-fourth to one-third fibers and tucked in a similar manner to a complete tuck, taking note not to restrict any elevation in adduction.
Harada-Ito Procedure
Originally described by Harada and Ito for extorsion,[46] it now encompasses any procedure that selectively strengthens the anterior half of the SO tendon. In the original approach, a suture was passed 3mm behind the insertion which was then anchored to the sclera 3mm anterior and lateral to SO insertion. Fells modified the technique in 1974.[47] This procedure has little effect on vertical deviation and does not cause iatrogenic Brown syndrome. It corrects up to 10 degrees of excyclotorsion in primary position and up to 15 to 20 degrees in downgaze.[48]
Access is gained to SO tendon as described above except that the incision is extended circumferentially in the temporal direction. After isolating the SO tendon, it is split into two up to midpoint of SR. A 6-0 absorbable suture is passed through the anterior portion, each end locked and the anterior portion is disinserted. It is then transposed anteriorly and laterally 8mm posterior to the LR insertion and just above the superior border of LR.
Management of SO Palsy
Based on the magnitude of hypertropia in different gazes, Knapp[49] and Knapp and Moore[41] classified the common presentations of SO palsy into seven classes. Based on this classification, Noorden et al[50] have advocated the surgical methods which are briefly summarized in Table 3. Whereas they advocated for IO myectomy, the preferred method for IO weaking is IO recessions as outlined above. Class 7 represents a peculiar case where classic SO palsy is associated with restriction of elevation in adduction (pseudo-Brown syndrome). This is attributed to direct trochlear damage due to dog bites or frontal sinus surgery.
| Class | Hypertropia in Diagnostic Position | Surgical Treatment |
|---|---|---|
| 1 | Levoelevation | RIO weakening (recession) |
| 2 | Levodepression | RSO tuck (8-12mm) ± LIR recession |
| 3 | All Levoversion Positions | Hypertropia ≤ 25Δ: RIO recession
Hypertropia > 25Δ: RIO recession + RSO tuck |
| 4 | All Levoversion and Downgazes | As in class 3 + RSR/LIR recession |
| 5 | All Downgazes | RSO tuck + RSR/LIR recession |
| 6 | Bilateral | Bilateral surgery |
| 7 | All Downgazes and Primary Position | Explore trochlea |
In classes 4 and 5, if forced duction of ipsilateral superior rectus is restricted, then recession of SR should be done. If SR ductions are full and free, then recession of contralateral inferior rectus should be preferred.
SO Weakening Procedures
The various conditions associated with SO overaction that may benefit from SO weakening procedures are as follows:
- A-pattern strabismus
- Brown’s syndrome
- IO palsy
- Superior oblique myokymia
SO Tenotomy/Tenectomy
After ensuring isolation of all fibres of the SO tendon, the SO tendon is divided (tenotomy) or a section is removed (tenectomy). The tendon is then allowed to retract. It can correct 20 Δ or more of A pattern in the primary position[51] and up to 45 Δ in downgaze.[52] Undercorrection is mainly due to incomplete tenotomy or tenectomy. The most common complication is iatrogenic SO palsy (overcorrection) and is seen in 30-85% of the cases.[53]
For superior oblique myokymia, a large tenectomy is necessary to avoid reattachment. To counter the resultant SO palsy, an IO weakening procedure is advocated at the same time.[54] Nasal transposition of anterior fibers of SO to selectively weaken intorsion has also been described.[55]
Posterior Tenotomy of Superior Oblique (PTSO)
This procedure selectively weakens the depression and abducting actions of the posterior fibres of SO while preserving the torsional action of the anterior fibres. After SO isolation under adequate visualization, the SO fibres are cut at the scleral insertion from a posterior approach sparing the anterior 1-2mm of the tendon.
Superior Oblique Expander
To avoid unpredictable overcorrection and excyclotorsion induced by SO tenotomy, SO can be weakened in a graded manner by expending the length of the tendon using a silicone spacer. After hooking the SO tendon, a double-armed nonabsorbable suture is passed through the tendon 2-3mm nasal to SR border and locked on each end. A similar suture is passed 2mm from the first one and the tendon is cut between the two. A silicone band (size 240, width 2.5mm) used for retinal buckling procedures is trimmed to the desired length (4-7mm) according to the degree of SO overaction. Each end of the nonabsorbable suture is passed through the band along its width. The sutures are tired to secure the expander to both ends of SO. Intraoperative exaggerated FDT is done to confirm the release of restriction in cases of Brown syndrome. The procedure causes very few complications the most common being undercorrection and persistent SO overaction.
Translational Recession
This procedure is indicated for severe SO overactions wherein the SO tendon is sutured 6mm nasal to SR and 12mm posterior to limbus. This prevents the limitation of depression in abduction seen in anterior placement of SO. However, the increased weakening of intorting action makes it a less physiological SO weakening procedure.[56]
Dissociated Vertical Deviation
DVD classically manifests as the upward deviation of either eye when the patient is fatigued, or fusion artificially interrupted by covering one eye. The upward movement is associated with extorsion and when the cover is removed, the eye moves downwards with intorsion to take up fixation. DVD is mostly bilateral but asymmetric. It is often associated with infantile esotropia and latent nystagmus. For details on pathogenesis, clinical features and diagnosis, refer to the sections on DVD under Hypertropia.
DVD that measures the same (±7Δ) in abduction, adduction and primary position is referred to as comitant DVD whereas incomitant DVD refers to different vertical deviations in these 3 positions.[57]
Management of DVD
Patients with DVD are mostly asymptomatic with infrequent complaints of diplopia. Aim of nonsurgical therapy for DVD is to strengthen the patient’s fusional mechanisms, elimination of any concurrent strabismus and optimization of vision through accurate refractive prescription and treatment of amblyopia. Indications for surgery are visual symptoms, physical discomfort from a large deviation, or cosmetic disfigurement.
The available options are as follows:
- Supramaximal Recession of Bilateral SR (7-10mm): This procedure yields the best results in cases of comitant bilateral DVD. In cases of asymmetric bilateral DVD (more than ±7Δ) in the two eyes, greater recession is done in eye with greater vertical deviation.[58]
- Retroequatorial Myopexy (Faden) of SR: This procedure is combined with SR recessions of smaller magnitude (3-5mm)
- Inferior rectus Resection (up to 4mm): Reserved for recurrent comitant DVD after maximum SR recession (10mm) have failed to correct vertical deviation
- IO weakening procedures: Incomitant DVD with greater vertical deviation in adduction and IOOA can be managed by anteropositioning of IO as it converts IO into a depressor. Combined SR recession with IO recession (8-10mm) are another option.
- SO weakening procedures: Incomitant DVD with greater vertical deviation in abduction, SO overaction and A-pattern are managed by combined SR recessions for vertical deviation and PTSO for SO overaction
- Horizontal Rectus Recessions: Combined with faden procedure, these are reserved for Dissociated horizontal deviations (LR recession for exo-DHD and MR recession for eso-DHD).
Monocular Elevation Deficit (Double Elevator Palsy)
Indications for surgery in this scenario include hypotropia in primary position or chin elevation or both. The aim of surgery is to restore binocular vision in primary position. The available surgical modalities are as follows:
- Knapp procedure:[59] (Figure 9) Transposition of horizontal recti to the insertion of superior rectus (or inferior rectus in case of double depressor palsy). This procedure is most beneficial when there is no IR contracture.
- IR recession: This is the procedure of choice in case the passive ductions for IR are restricted indicating contracture. In some cases, both the modalities might be necessary.
- Contralateral SR recession: This might be used as a supplementary procedure to IR recession in case of large vertical deviations.
Transposition of Cyclovertical Muscles
The effect of transposition of muscles is due to the shift in the vector forces to the new insertion site,[60] rather than relearning of the muscle function as was initially postulated. They result in improved saccadic velocities though not to normal levels. The various indications for transposition of cyclovertical muscles and the procedures involved are outlined below.
A-V Pattern Strabismus
Horizontal transposition of vertical recti has been shown to be effective for management of A-V patterns except A-exotropia.[61] For A-esotropia and V-esotropia, SR and IR respectively are transposed 7mm temporally. This leads to increase in abductive action for SR in upgaze and for IR in downgaze. For V-exotropia, SR is shifted 7mm nasally. However, vertical transposition of horizontal recti is the preferred procedure for A-V patterns (with no oblique overactions) due to better correction of deviation in the primary position.
Horizontal Strabismus
For residual tropias after surgery on all horizontal recti, temporal transposition of vertical recti for esotropia and nasal transposition for exotropia has been described.[62] 5mm transposition of both SR and IR corrected 10-14 Δ whereas 7-8 mm displacement of both resulted in correction of 25Δ.
Cyclotropias
For correction of cyclovertical deviations without producing the undesirable vertical effect, conventional oblique weakening procedures cannot be used. Harada-Ito procedure can be used in this case for correction of excyclotropia.[46] Also, nasal shifting of IR and temporal shifting of SR will correct excyclotropia and vice versa for incyclotropia.[63]
VI Nerve Palsy
Transposition procedures are best suited for patients with weak LR force generation and a saccadic velocity <100°/sec.[39] Conventional LR resection is indicated in other cases.
Hummelsheim’s Partial Tendon Transposition[64]
This was the first description of a transposition procedure for a paralytic LR muscle. In this procedure, the lateral halves of SR and IR are transposed to LR insertion (Figure 10)
O’Connor's Transposition Procedure
Initially he advocated full tendon transposition[65] but due to vertical imbalance, he shifted to partial tendon transposition where he transposed the nasal halves of SR and IR to LR to decrease adducting power while increasing abduction.
Jenson’s Rectus Muscle Reunion[66]
SR, IR and LR are split along their long axis and the lateral halves of SR and IR are sutured to the superior and inferior half of LR respectively. MR recession can be added as a supplementary procedure (Figure 11).
Adjustable Transposition
SR and IR are isolated and disinserted. They are sutured 1mm above and below LR insertion respectively with their long axis aligned with LR. The sutures are tied in a slipknot manner and conjunctiva left often for postoperative adjustments.[39]
Nishida's Procedure[67]
SR and IR tendons are split from the center of insertion to 15mm posteriorly and the lateral halves are fixed with anchoring sutures onto the sclera 8mm posterior to the superior and inferior border of LR respectively (Figure 12A). There is no vertical muscle tenotomy as in Hummelsheim’s procedure or LR splitting and transposition as in Jensen’s procedure. A modification of this procedure was subsequently published which did not require muscle splitting.[68] The temporal margin of each vertical rectus was transposed supero- or infero-temporally 10-12mm posterior to limbus and anchored onto the sclera using non-absorbable sutures (Figure 12B).
III Nerve Palsy
In a complete third nerve palsy, the only cyclovertical muscle that can provide adducting force is the Superior Oblique.
SO Transposition
In the original descriptions of using SO as an internal rotator in IIIrd nerve palsy,[69] fracture of trochlea was necessary which was technically difficult and cumbersome for both the surgeon and the patient. Scott advocated anterior transposition of SO without trochleotomy.[70] The SO tendon is shifted 2mm nasal and anterior to nasal border of SR without trochlear fracture. By adding resection of SO and transposing the tendon to the MR, the SO functions of depression, abduction, and intorsion are converted to mild adduction.
For complications related to strabismus surgery, refer to the section on Strabismus Surgery complications.
References
- ↑ Scobee RG. Esotropia: Incidence, etiology and results of therapy. Am J Ophthalmol. Published online 1951:34:817.
- ↑ Sharma K, Abdul-Rahim AS. Vertical fusion amplitude in normal adults. Am J Ophthalmol. 1992;114(5):636-637. doi:10.1016/s0002-9394(14)74499-x
- ↑ Ozsoy E, Gunduz A, Ozturk E. Inferior Oblique Muscle Overaction: Clinical Features and Surgical Management. J Ophthalmol. 2019;2019:9713189
- ↑ Wolff J. The occurrence of retraction movements of the eyeball together with congenital defects in the external ocular muscles. Arch Ophthalmol. Published online 1900:29:297
- ↑ Knapp P. Discussion of: Quantitative forced duction by KF Stephens and R Reinecke. Trans Am Acad Ophthalmol Otolaryngol. Published online 1967:71:329
- ↑ Guyton DL. Exaggerated traction test for the oblique muscles. Ophthalmology. 1981;88(10):1035-1040. doi:10.1016/s0161-6420(81)80033-4
- ↑ 7.0 7.1 Long-term follow-up of bilateral botulinum toxin injections versus bilateral recessions of the medial rectus muscles for treatment of infantile esotropia - PubMed. Accessed May 24, 2023. https://pubmed.ncbi.nlm.nih.gov/22681945/
- ↑ McNeer KW, Tucker MG, Guerry CH, Spencer RF. Incidence of stereopsis after treatment of infantile esotropia with botulinum toxin A. J Pediatr Ophthalmol Strabismus. 2003;40(5):288-292. doi:10.3928/0191-3913-20030901-10
- ↑ Etezad Razavi M, Sharifi M, Armanfar F. Efficacy of botulinum toxin in the treatment of intermittent exotropia. Strabismus. 2014;22(4):176-181. doi:10.3109/09273972.2014.962750
- ↑ Scott AB, Kraft SP. Botulinum toxin injection in the management of lateral rectus paresis. Ophthalmology. 1985;92(5):676-683. doi:10.1016/s0161-6420(85)33982-9
- ↑ Holmes JM, Droste PJ, Beck RW. The natural history of acute traumatic sixth nerve palsy or paresis. J AAPOS Off Publ Am Assoc Pediatr Ophthalmol Strabismus. 1998;2(5):265-268. doi:10.1016/s1091-8531(98)90081-7
- ↑ Akbari MR, Ameri A, Keshtkar Jaafari AR, Mirmohammadsadeghi A. Botulinum toxin injection for restrictive myopathy of thyroid-associated orbitopathy: success rate and predictive factors. J AAPOS Off Publ Am Assoc Pediatr Ophthalmol Strabismus. 2016;20(2):126-130.e1. doi:10.1016/j.jaapos.2016.01.007
- ↑ Talebnejad MR, Tahamtan M, Nowroozzadeh MH. Botulinum Toxin Injection for Treatment of Acute Traumatic Superior Oblique Muscle Palsy. J Ophthalmic Vis Res. 2015;10(3):263-267. doi:10.4103/2008-322X.170350
- ↑ Barry JS, Dawson ELM, Adams GGW, Lee JP. Role of inferior rectus botulinum toxin injection in iatrogenic vertical strabismus. Strabismus. 2011;19(2):38-42. doi:10.3109/09273972.2011.575433
- ↑ Bunting HJ, Dawson ELM, Lee JP, Adams GGW. Role of inferior rectus botulinum toxin injection in vertical strabismus resulting from orbital pathology. Strabismus. 2013;21(3):165-168. doi:10.3109/09273972.2013.811602
- ↑ Stager D Jr, Dao LM, Felius J. Uses of the Inferior Oblique Muscle in Strabismus Surgery. Middle East Afr J Ophthalmol. 2015 Jul-Sep;22(3):292-7. doi: 10.4103/0974-9233.159723. PMID: 26180466; PMCID: PMC4502171.
- ↑ Jin ZW, Umeki S, Takeuchi Y, Yamamoto M, Murakami G, Abe S, Rodríguez-Vázquez JF. Inferior oblique muscle of the eye: its foetal development with special reference to understanding of the frequent variants in adults. Folia Morphol (Warsz). 2022;81(2):442-450. doi: 10.5603/FM.a2021.0043. Epub 2021 May 6. PMID: 33954958
- ↑ Sanjari MS, Shahraki K, Nekoozadeh S, Tabatabaee SM, Shahraki K, Aghdam KA. Surgical treatments in inferior oblique muscle overaction. J Ophthalmic Vis Res. 2014 Jul-Sep;9(3):291-5. doi: 10.4103/2008-322X.143355. PMID: 25667727; PMCID: PMC4307652.
- ↑ 19.0 19.1 Parks MM. A study of the weakening surgical procedures for eliminating overaction of the inferior oblique. Trans Am Ophthalmol Soc. 1971;69:163-187
- ↑ 20.0 20.1 Parks MM. The weakening surgical procedures for eliminating overaction of the inferior oblique muscle. Am J Ophthalmol. 1972;73(1):107-122. doi:10.1016/0002-9394(72)90313-3
- ↑ 21.0 21.1 Sefi-Yurdakul N, Gucyetmez V. Inferior Oblique Overaction: The Results of Myectomy in Cases with a Primary Position Vertical Deviation Less and More Than 20 Prism Diopters. Middle East Afr J Ophthalmol. 2020 Jul 20;27(2):117-122. doi: 10.4103/meajo.MEAJO_150_19. PMID: 32874045; PMCID: PMC7442083.
- ↑ Surgery on the Inferior Oblique Muscle. In: Strabismus Surgery and its Complications. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-32704-2_11
- ↑ Fink, W.H. Surgery of the Vertical Muscles of the Eye. 2nd ed. Springfield, Charles C Thomas; 1962
- ↑ 24.0 24.1 24.2 24.3 Apt L, Call NB. Inferior oblique muscle recession. Am J Ophthalmol. 1978;85(1):95-100. doi:10.1016/s0002-9394(14)76672-3
- ↑ Ziffer AJ, Isenberg SJ, Elliott RL, Apt L. The effect of anterior transposition of the inferior oblique muscle. Am J Ophthalmol. 1993;116(2):224-227. doi:10.1016/s0002-9394(14)71290-5
- ↑ Huang Y-T, Chen JJ-Y, Wu M-Y, Tien P-T, Tsui Y-P, Hsieh Y-C, Lin H-J, Wan L. The Effects of Modified Graded Recession, Anteriorization and Myectomy of Inferior Oblique Muscles on Superior Oblique Muscle Palsy. Journal of Clinical Medicine. 2021; 10(19):4433. https://doi.org/10.3390/jcm10194433.
- ↑ Stager DR, Weakley DR, Stager D. Anterior transposition of the inferior oblique. Anatomic assessment of the neurovascular bundle. Arch Ophthalmol Chic Ill 1960. 1992;110(3):360-362. doi:10.1001/archopht.1992.01080150058028
- ↑ Gobin MH. ANTEROPOSITION OF THE INFERIOR OBLIQUE MUSCLE IN V-ESOTROPIA. Ophthalmol J Int Ophtalmol Int J Ophthalmol Z Augenheilkd. 1964;148:325-341. doi:10.1159/000304704
- ↑ Elliott RL, Nankin SJ. Anterior transposition of the inferior oblique. J Pediatr Ophthalmol Strabismus. 1981;18(3):35-38. doi:10.3928/0191-3913-19810501-08
- ↑ Kushner BJ. Restriction of elevation in abduction after inferior oblique anteriorization. J AAPOS Off Publ Am Assoc Pediatr Ophthalmol Strabismus. 1997;1(1):55-62. doi:10.1016/s1091-8531(97)90024-0
- ↑ Prakash P, Gupta A, Sharma P. Pure anteropositioning of inferior oblique. A selective weakening procedure. Acta Ophthalmol (Copenh). 1994;72(3):373-375. doi:10.1111/j.1755-3768.1994.tb02776.x
- ↑ Moon K, Lee SY. The effect of graded recession and anteriorization on unilateral superior oblique palsy. Korean J Ophthalmol. 2006 Sep;20(3):188-91. doi: 10.3341/kjo.2006.20.3.188. PMID: 17004635; PMCID: PMC2908845.
- ↑ Stager DR, Beauchamp GR, Wright WW, Felius J, Stager D. Anterior and nasal transposition of the inferior oblique muscles. J AAPOS Off Publ Am Assoc Pediatr Ophthalmol Strabismus. 2003;7(3):167-173. doi:10.1016/s1091-8531(03)00003-x
- ↑ 34.0 34.1 Stager DR Jr, Wang X, Stager DR Sr, Beauchamp GR, Felius J. Nasal myectomy of the inferior oblique muscles for recurrent elevation in adduction. J AAPOS. 2004 Oct;8(5):462-5. doi: 10.1016/j.jaapos.2004.07.004. PMID: 15492740.
- ↑ Kızıltoprak H, Yaşar HH, Tekin K. The Effect of Inferior Oblique Muscle Z-Myotomy in Patients with Primary Inferior Oblique Overaction. Turk J Ophthalmol. 2020 Apr 29;50(2):82-86. doi: 10.4274/tjo.galenos.2019.87947. PMID: 32367698; PMCID: PMC7204901.
- ↑ Karam M, Alsaif A, Alhajeri S, et al. Inferior Oblique Anterior Transposition versus Myectomy for Inferior Oblique Overaction: Systematic Review and Meta Analysis. Eur J Ophthalmol. Published online September 21, 2022:11206721221127768. doi:10.1177/11206721221127769
- ↑ Stager DR. The neurofibrovascular bundle of the inferior oblique muscle as its ancillary origin. Trans Am Ophthalmol Soc. 1996;94:1073-1094
- ↑ Del Monte MA, Parks MM. Denervation and extirpation of the inferior oblique. An improved weakening procedure for marked overaction. Ophthalmology. 1983;90(10):1178-1185. doi:10.1016/s0161-6420(83)34409-2
- ↑ 39.0 39.1 39.2 Rosenbaum AL, Santiago AP. Clinical Strabismus Management: Principles and Surgical Techniques. WB Saunders; 1999.
- ↑ Niyaz L, Yücel OE, Gul A. Infrequent Complications of Inferior Oblique Recession Surgery. Semin Ophthalmol. 2017;32(5):593-596. doi: 10.3109/08820538.2015.1132332. Epub 2016 May 18. PMID: 27191970.
- ↑ 41.0 41.1 Knapp P, Moore S. Diagnosis and surgical options in superior oblique surgery. Int Ophthalmol Clin. 1976;16(3):137-149.
- ↑ Morris RJ, Scott WE, Keech RV. Superior oblique tuck surgery in the management of superior oblique palsies. J Pediatr Ophthalmol Strabismus. 1992;29(6):337-346; discussion 347-348. doi:10.3928/0191-3913-19921101-04
- ↑ Saunders RA. Treatment of superior oblique palsy with superior oblique tendon tuck and inferior oblique muscle myectomy. Ophthalmology. 1986;93(8):1023-1027. doi:10.1016/s0161-6420(86)33627-3
- ↑ Pineles SL, Velez FG. Anterior superior oblique tuck: an alternate treatment for excyclotorsion. J AAPOS. 2018;22(5):393-393.e1. doi:10.1016/j.jaapos.2018.05.019
- ↑ Solanes F, Velez FG, Robbins L, Pineles SL. Modified Anterior Superior Oblique Tuck: A Case Series. J Binocul Vis Ocul Motil. 2020;70(4):157-162. doi:10.1080/2576117X.2020.1801033
- ↑ 46.0 46.1 Harada M, Ito Y. Surgical correction of cyclotropia. Jpn J Ophthalmol. Published online 1964:8:88
- ↑ Fells P. Management of paralytic strabismus. Br J Ophthalmol. 1974;58(3):255-265.
- ↑ Mitchell PR, Parks MM. Surgery of bilateral superior oblique palsy. Ophthalmology. 1982;89(5):484-488. doi:10.1016/s0161-6420(82)34765-x
- ↑ Knapp P. First Annual Richard G. Scobee Memorial Lecture. Diagnosis and surgical treatment of hypertropia. Am Orthopt J. 1971;21:29-37.
- ↑ 50.0 50.1 von Noorden GK, Murray E, Wong SY. Superior oblique paralysis. A review of 270 cases. Arch Ophthalmol Chic Ill 1960. 1986;104(12):1771-1776. doi:10.1001/archopht.1986.01050240045037
- ↑ Parks MM. Management of overacting superior oblique muscles. Trans New Orleans Acad Ophthalmol. 1986;34:409-418.
- ↑ Scott WE, Jampolsky AJ, Redmond MR. Superior oblique tenotomy: indications and complications. Int Ophthalmol Clin. 1976;16(3):151-159.
- ↑ von Noorden GK, Olivier P. Superior oblique tenectomy in Brown’s syndrome. Ophthalmology. 1982;89(4):303-309. doi:10.1016/s0161-6420(82)34787-9
- ↑ Brazis PW, Miller NR, Henderer JD, Lee AG. The natural history and results of treatment of superior oblique myokymia. Arch Ophthalmol Chic Ill 1960. 1994;112(8):1063-1067. doi:10.1001/archopht.1994.01090200069025
- ↑ Kosmorsky GS, Ellis BD, Fogt N, Leigh RJ. The treatment of superior oblique myokymia utilizing the Harada-Ito procedure. J Neuro-Ophthalmol Off J North Am Neuro-Ophthalmol Soc. 1995;15(3):142-146
- ↑ Sharma P, Thanikachalam S, Kedar S, Bhola R. Evaluation of subjective and objective cyclodeviation following oblique muscle weakening procedures. Indian J Ophthalmol. 2008;56(1):39-43
- ↑ McCall LC, Rosenbaum AL. Incomitant dissociated vertical deviation and superior oblique overaction. Ophthalmology. 1991;98(6):911-917; discussion 917-918. doi:10.1016/s0161-6420(91)32202-4
- ↑ Magoon E, Cruciger M, Jampolsky A. Dissociated vertical deviation: an asymmetric condition treated with large bilateral superior rectus recession. J Pediatr Ophthalmol Strabismus. 1982;19(3):152-156. doi:10.3928/0191-3913-19820501-09
- ↑ Knapp P. The surgical treatment of double-elevator paralysis. Trans Am Ophthalmol Soc. 1969;67:304-323.
- ↑ Metz HS, Scott AB. Innervational plasticity of the oculomotor system. Arch Ophthalmol Chic Ill 1960. 1970;84(1):86-91. doi:10.1001/archopht.1970.00990040088021
- ↑ Miller JE. Vertical recti transplantation in the A and V syndromes. Arch Ophthalmol Chic Ill 1960. 1960;64:175-179. doi:10.1001/archopht.1960.01840010177002
- ↑ Nawratzki I, Benezra D. Transposition of vertical recti for residual tropias. Ann Ophthalmol. 1976;8(10):1245-1250
- ↑ von Noorden GK, Chu MW. Surgical treatment options in cyclotropia. J Pediatr Ophthalmol Strabismus. 1990;27(6):291-293. doi:10.3928/0191-3913-19901101-05
- ↑ Hummelsheim E. Weitere Erfahrungen mit partieller Sehnenuberpflanzung an den Augenmuskeln. Arch Augenheilkd. 1908;62:71-4
- ↑ O’Connor R. Transplantation of ocular muscles. American Journal of Ophthalmology. 1921 Nov 1;4(11):838-45.
- ↑ Jensen CD. RECTUS MUSCLE UNION: A NEW OPERATION FOR PARALYSIS OF THE RECTUS MUSCLES. Trans Pac Coast Otoophthalmol Soc Annu Meet. 1964;45:359-387.
- ↑ Nishida Y, Inatomi A, Aoki Y, et al. A muscle transposition procedure for abducens palsy, in which the halves of the vertical rectus muscle bellies are sutured onto the sclera. Jpn J Ophthalmol. 2003;47(3):281-286. doi:10.1016/s0021-5155(03)00021-2
- ↑ Nishida Y, Hayashi O, Oda S, et al. A simple muscle transposition procedure for abducens palsy without tenotomy or splitting muscles. Jpn J Ophthalmol. 2005;49(2):179-180. doi:10.1007/s10384-004-0151-2
- ↑ Jackson E. Cited in: Wiener, M, Scheie HG, eds. Surgery of the Eye, 3rd ed. New York: Grune & Stratton, 1952; 405.
- ↑ Scott AB. Transposition of the superior oblique. Am Orthopt J. 1977;27:11-14.