Heavy Eye Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
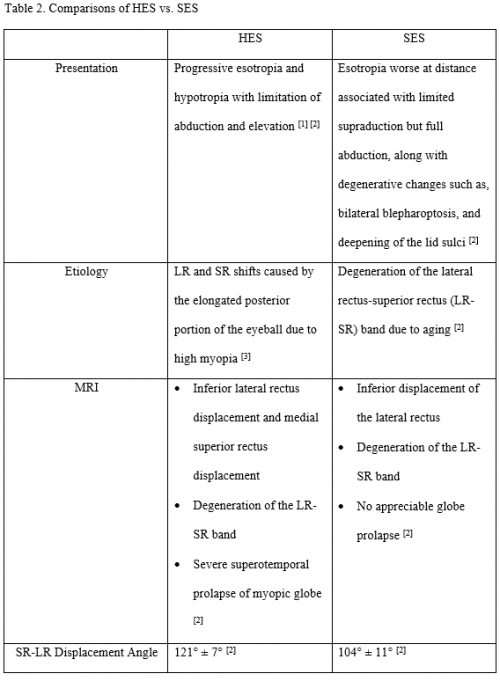
Heavy eye syndrome (HES), also called Strabismus fixus convergence, myopic strabismus fixus, and highly myopic strabismus, is a cause of acquired strabismus in the setting of high myopia. Patients classically present with diplopia secondary to progressive esotropia and hypotropia with limitation of abduction and elevation, although exotropia and hypertropia have also been described.[1][2] Heavy eye syndrome should be differentiated from sagging eye syndrome (SES) which is mostly seen in non-myopic elderly population and presents with esotropia worse at distance along with degenerative changes such as, bilateral blepharoptosis, and deepening of the lid sulci.[2]
Etiology
Heavy eye syndrome was originally thought to result from the gravitational pull downward from a heavy eye.[3] It is hypothesized that HES is the result of lateral rectus (LR) and superior rectus (SR) shifts caused by the prolapse out of the muscle cone of the elongated posterior portion of the eyeball due to axial elongation in high myopia.[4] The prolapse typically occurs in the superotemporal quadrant, which may be particularly susceptible due to age-related changes,[5] leading to inferior displacement of the lateral rectus and medial displacement of the superior rectus. Inferior shift of the LR causes reduced supraduction. Nasal shift of the SR causes reduced abduction. Consequently, HES shows esodeviation and hypodeviation with limitation of abduction and supraduction.[6]
Epidemiology
Most have a refractive error of greater than -12.00 D and an axial length of greater than 25 mm. [7][8] In Japanese patients with ≥6.00 D of refractive error or an axial length ≥27 mm, the prevalence of HES was 2.65%.[9] A large multicenter study of patients with heavy eye syndrome in Germany and Switzerland reported by Wabbels et al found a mean age of 59.7 years (range 16-87 years), with patients typically presenting at 40 years or later.[7] Seventy-five percent of the Wabbels et al cohort was comprised of women.[7]
Diagnosis
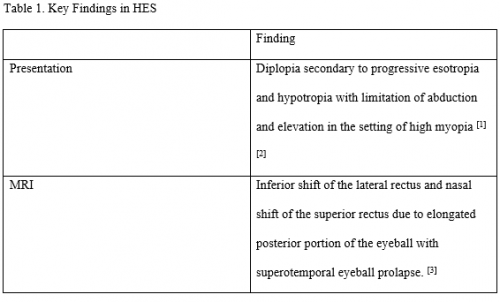
There are no definitive diagnostic criteria for HES;[6] however, findings are described below. Table 1 compiles key findings in HES.
History
Heavy eye syndrome is not typically seen in childhood. Patients typically have high myopia. Some patients will complain of new onset diplopia in adulthood.[10] Some patients may present with concerns about appearance of the eye.[11] The older and more myopic the patient, the more likely the patient will have an acquired esotropia and/or a vertical heterotropia.[12]
Clinical Findings
Patients typically have high myopia. Average axial length in patients with HES is reportedly between 28.9 mm[9] and 31.4 mm.[13]
MRI (magnetic resonance imaging) findings
Neuroimaging, preferably with MRI, can help evaluate the paths of the rectus muscles and show superotemporal prolapse of the myopic globe.[1] [14][8] If altered paths of the muscles are noted, the surgical options will aim to correct the deviation. High resolution MRI may also show thinning, elongation, or rupture of the LR-SR intermuscular septum.[2] If no abnormality is found and in the absence of other causes, classical recession-resection surgery may be beneficial.[1]
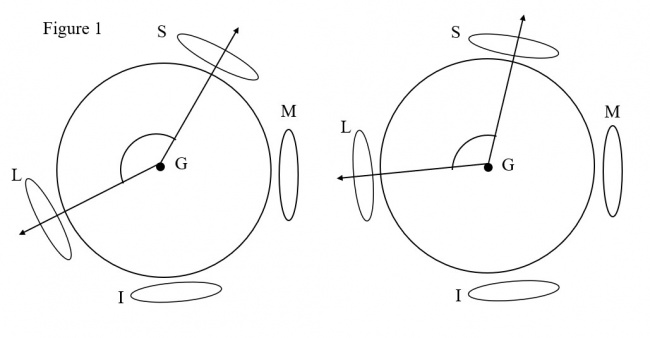
Yamaguchi et al. investigated the anatomic relationships between the globe, SR, and LR muscles with coronal MRI. The angle formed by the globe, LR, and SR was calculated and referred to as the angle of dislocation of the globe.[15] Their study found patients with highly myopic strabismus to have a mean angle of dislocation of 179.9° ± 30.8° while in the control group the mean angle of dislocation was 102.9° ± 6.8° (P < .001).[15] This finding is represented by Figure 1.
Tan et al. measured this angle in HES vs SES patients. The mean angle between the lateral rectus and superior rectus muscles in HES was 121° ± 7° while in SES, the mean angle between the lateral rectus and superior rectus muscles was 104° ± 11°, significantly less than in HES (P < 0.001) [2].
Complications
Mansour et al. reported two cases of acquired convergent strabismus fixus that developed ocular ischemia, atrophy of the optic nerve, and central retinal artery occlusion. They believed these complications to be secondary to mechanical stretching and torsion of the optic nerve with subsequent strangulation of its blood supply. They recommended early surgical correction of strabismus fixus.[16]
Differential diagnosis
- Endocrine ophthalmopathy [17]
- Sagging Eye Syndrome [2]
- Uncorrected hyperopic refractive error [18]
- High accommodative convergence/accommodation ratio [18]
- Duane syndrome [18]
- Myasthenia gravis [18]
- Thyroid eye disease
- Cranial nerve palsy (Third, fourth, or sixth nerves)
In patients with highly myopic strabismus, it is important to distinguish HES from SES as the distinction drives appropriate surgery. There is overlap of motility findings; therefore, imaging should be obtained. Orbital MRI demonstrates inferior lateral rectus displacement and medial superior rectus displacement with severe superotemporal prolapse of the myopic globe in HES, whereas only inferior displacement of the lateral rectus results from degeneration of the LR-SR band is seen in SES.[2] Distinctions and similarities have been compiled into Table 2.
Management
Surgery
Recession-Resection
Hayashi et al. found the recession and resection (R&R) procedure to be easy and effective when the abducting disorder is not severe. However, R&R was less successful in patients with more severe disease, which they defined as cases where the patient could not abduct to the midline or had a fixed eyeball in the extreme adducting position.[10]
Loop Myopexy
The most successful outcomes have come from correcting the muscle paths of both the superior and lateral rectus muscles. The most commonly performed surgery involves loop myopexy of the superior and lateral rectus muscles either with or without muscles splitting.[1] Yamaguchi et al. demonstrated the efficacy of loop myopexy±medial rectus recession in 23 patients. They were successful in decreasing the angle of dislocation of the globe, increasing the angles of maximum abduction and sursumduction, and decreasing the angle of ocular deviation. All 23 patients had positive forced duction tests preoperatively; and postoperatively, only 1 patient had a positive forced duction test. Dislocation of the globe, restriction of ocular movements, and ocular deviation did not relapse during follow up (mean 48.8 months).[15] Akbari et al. modified this procedure by using two sutures for muscle belly union which resulted in favorable outcomes in 16 patients. [19] Larsen and Gole proposed use of a Jensen's procedure with splitting of the lateral and superior rectus muscles and suturing together the superior half of the lateral rectus and temporal half of the superior rectus 15 mm from the limbus.[20] Silva et al. modified the loop myopexy with muscle splitting and scleral fixation.[21] The Yamada procedure describes that transposition of the superior half of the lateral rectus and temporal half of the superior rectus to a point half way in between these muscles along the spiral of Tillaux, often in conjunction with a medial rectus recession.[22] Awadein et al. described a "zip up" loop myopexy in which the lateral rectus and superior rectus are sutured 4-5 mm from their insertions with subsequent sutures connecting the superior and lateral rectus about every 3 mm, until no further sutures can be placed.[23] While many experts have performed medial rectus recession at the same time as loop myopexy, Bansal et al. demonstrated the efficacy of loop myopexy alone. In their case series, 21/29 (72%) did not require medial rectus recession and had a successful outcome with loop myopexy alone. A combined approach eliminates the need for a second procedure, while a staged approach reduces the overall amount of surgery required.[11]
References
- ↑ 1.0 1.1 1.2 1.3 Ranka M, Steele M. Esotropia associated with high myopia. - PubMed - NCBI. https://www.ncbi.nlm.nih.gov/pubmed/26247133. Accessed February 13, 2020.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Tan RJD, Demer JL. Heavy eye syndrome versus sagging eye syndrome in high myopia. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2015;19(6):500-506. doi:10.1016/j.jaapos.2015.08.012
- ↑ Pineles SL. Acquired Diplopia in Adults: Heavy Eye Syndrome. J Binocul Vis Ocul Motil. 2022 Oct-Dec;72(4):223-225. PMID: 36279483; PMCID: PMC9608378.
- ↑ Yamaguchi M, Yokoyama T, Shiraki K. Surgical procedure for correcting globe dislocation in highly myopic strabismus. Am J Ophthalmol. 2010 Feb;149(2):341-346.e2. doi: 10.1016/j.ajo.2009.08.035. Epub 2009 Nov 24. PMID: 19939345.
- ↑ Rutar T, Demer JL. "Heavy Eye" syndrome in the absence of high myopia: A connective tissue degeneration in elderly strabismic patients. J AAPOS. 2009 Feb;13(1):36-44. doi: 10.1016/j.jaapos.2008.07.008. Epub 2008 Oct 18. PMID: 18930668; PMCID: PMC2728014.
- ↑ 6.0 6.1 Aoki Y, Nishida Y, Hayashi O, et al. Magnetic resonance imaging measurements of extraocular muscle path shift and posterior eyeball prolapse from the muscle cone in acquired esotropia with high myopia. American Journal of Ophthalmology. 2003;136(3):482-489.
- ↑ 7.0 7.1 7.2 Wabbels B, Fricke J, Schittkowski M, et al. Yokoyama procedure for esotropia associated with high myopia: real-world data from a large-scale multicentre analysis. Acta Ophthalmol. Mar 02 2021;doi:10.1111/aos.14808
- ↑ 8.0 8.1 Tan RJ, Demer JL. Heavy eye syndrome versus sagging eye syndrome in high myopia. J AAPOS. Dec 2015;19(6):500–6. doi:10.1016/j.jaapos.2015.08.012 [PubMed: 26691027]
- ↑ 9.0 9.1 Nakao Y, Kimura T. Prevalence and anatomic mechanism of highly myopic strabismus among Japanese with severe myopia. Jpn J Ophthalmol. 2014 Mar;58(2):218-24. doi: 10.1007/s10384-013-0296-y. Epub 2014 Jan 7. PMID: 24390603.
- ↑ 10.0 10.1 Hayashi T, Iwashige H, Maruo T. Clinical features and surgery for acquired progressive esotropia associated with severe myopia. Acta Ophthalmol Scand. 1999;77(1):66-71. doi:10.1034/j.1600-0420.1999.770115.x
- ↑ 11.0 11.1 Bansal S MI. Unaugmented Muscle Union Surgery for Heavy Eye Syndrome Without Combined Medial Rectus Recession. - PubMed - NCBI. https://www.ncbi.nlm.nih.gov/pubmed/26836002.
- ↑ Rovick LP. Evaluation of Vertical Deviations Secondary to Anatomical Abnormalities. American Orthoptic Journal. 2011;61(1):34-38. doi:10.3368/aoj.61.1.34
- ↑ Krzizok TH, Schroeder BU. Measurement of recti eye muscle paths by magnetic resonance imaging in highly myopic and normal subjects. Invest Ophthalmol Vis Sci. 1999 Oct;40(11):2554-60. PMID: 10509649.
- ↑ Maiolo C, Fresina M, Campos EC. Role of magnetic resonance imaging in heavy eye syndrome. Eye. 2017;31(8):1163-1167. doi:10.1038/eye.2017.48
- ↑ 15.0 15.1 15.2 Yamaguchi M, Yokoyama T, Shiraki K. Surgical Procedure for Correcting Globe Dislocation in Highly Myopic Strabismus. American Journal of Ophthalmology. 2010;149(2):341-346.e2. doi:10.1016/j.ajo.2009.08.035
- ↑ Mansour AM, Wang F, el-Baba F, Henkind P. Ocular complications in strabismus fixus convergens. Ophthalmologica. 1987;195(3):161-166. doi:10.1159/000309806
- ↑ Demer JL, von Noorden GK. High myopia as an unusual cause of restrictive motility disturbance. Survey of Ophthalmology. 1989;33(4):281-284. doi:10.1016/0039-6257(82)90154-0
- ↑ 18.0 18.1 18.2 18.3 Rutstein R. Care of the Patient with Strabismus: Esotropia and Exotropia. https://www.aoa.org/documents/optometrists/CPG-12.pdf. Accessed February 19, 2020.
- ↑ Akbari MR, Bayat R, Mirmohammadsadeghi A, Inanloo B, Mirshahi R. Surgical outcome of a new modification to muscle belly union surgery in heavy eye syndrome. Strabismus. 2018;26(4):198-202. doi:10.1080/09273972.2018.1502793
- ↑ Larsen PC, Gole GA. Partial Jensen's procedure for the treatment of myopic strabismus fixus. J AAPOS. 2004 Aug;8(4):393-5. doi: 10.1016/j.jaapos.2004.04.002. PMID: 15314605.
- ↑ Silva AR, Mota Á, Lemos JA, Ribeiro I, Correia Barbosa R, Viana AR, Francisco C, Ferreira I, Breda J, Tenedório P. Surgical treatment outcomes in heavy eye syndrome - a case series. Strabismus. 2024 Jun;32(2):115-120. doi: 10.1080/09273972.2024.2358074. Epub 2024 May 27. PMID: 38801053.
- ↑ Yamada M, Taniguchi S, Muroi T, Satofuka S, Nishina S. Rectus eye muscle paths after surgical correction of convergent strabismus fixus. Am J Ophthalmol. 2002 Oct;134(4):630-2. doi: 10.1016/s0002-9394(02)01587-8. PMID: 12383836.
- ↑ Awadein A, Farag CS, Maher S. Zip-up Loop Myopexy in Heavy Eye Syndrome. J Pediatr Ophthalmol Strabismus. 2024 Jul-Aug;61(4):279-286. doi: 10.3928/01913913-20240219-01. Epub 2024 Mar 14. PMID: 38482802.