Commotio Retinae
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Commotio retinae refers to traumatic retinopathy secondary to direct or indirect trauma to the globe. Retinopathy may be present at areas of scleral impact (coup) and or distant sites (contrecoup) including the macula. Commotio retinae in the posterior pole is also referred to as Berlin's edema.[1]
Etiology
Commotio retinae is caused by closed globe trauma or blast injury and is present in about 30% of all eye traumas presenting for hospital treatment.[2]
Risk Factors
Risk factors include high-impact sports activities (most commonly ball sports), violence, motor vehicle accidents, and other activities associated with blunt trauma to the face and orbits.
General Pathology
Retinal whitening in commotio retinae always involves loss or disruption of the photoreceptor outer segments but may also include damage to additional retinal layers.[3][4] Choroidal thickening is noted as well and can be visualized with enhanced-depth imaging OCT. Burke et al hypothesized choroidal vascular dilation in response to trauma may be the reason for increased choroidal thickness.[5]
Pathophysiology
Blunt trauma causes displacement of the lens–iris diaphragm with outward expansion of peripheral structures. Indirect injuries, such as blast trauma or orbital trauma, transmit shockwaves to the globe causing similar deformation-related force injuries.[2] This causes stretching and tearing of ocular tissues secondary to the vitreoretinal deformation caused by transmission of hydraulic forces.[2][6] The inelastic retina absorbs the full effect of shock waves, resulting in injury to various layers but mainly the outer segment of the photoreceptor and retinal pigment epithelium (RPE) junction.[7] It has been postulated that the injury is most severe at the photoreceptor processes, rather than in the remainder of the neurosensory retina, as these processes are not suspended by the Muller cells.[6]
There is no significant breakdown of the blood–retina barrier associated with commotio retinae.[3] While the retinal blood flow does not appear to be altered, the choroidal circulation may be impaired.[8][9]
Mansour et al documented disruption of photoreceptor outer segments, deposition of debris in the subretinal space, and RPE cell injury in a cadaveric human eye processed within 24 hours of trauma.[6] The characteristic glistening appearance they described is likely related to increased scattering of light by the abnormal photoreceptor processes and subretinal debris, which is well characterized by OCT.[4][8]
Restoration of photoreceptor outer segments begins at around 1 week and continues for at least 2 months, which may explain the course of visual acuity recovery.[3] The clinical appearance of commotio retinae resolves within 1 week, with restoration of normal fundus appearance or pigmentary changes dependent on the severity of the injury.[4]
Primary Prevention
Primary prevention includes the use of protective eye wear for athletes. Two-millimeter polycarbonate lenses in normal streetwear are recommended for low-impact sports, while impact-resistant sports frames with a 3-mm polycarbonate lens are recommended for moderate-to-high impact sports. Face masks attached to a helmet should be used in the highest risk sports, such as ice hockey, field hockey, football, baseball, and lacrosse.[10]
Diagnosis
Diagnosis is clinical and is made based on the characteristic appearance of commotio retinae on exam. OCT usually shows hyperreflectivity of the ellipsoid layer.[11]
History
Patients or bystanders will often offer a mechanism of trauma. It is important to screen for child abuse and domestic abuse as indicated.
Physical Examination
A complete ophthalmoscopic exam to rule out open globe injury and orbital fracture, including dilated fundus examination, is indicated after significant trauma.
Signs
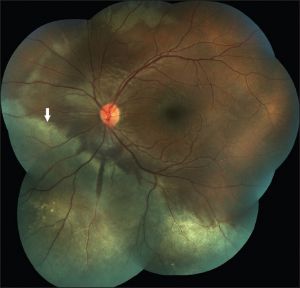
Dilated funduscopic exam reveals glistening gray-white opacification of the neurosensory retina with or without intraretinal hemorrhages and RPE mottling (Figure 1).[2] A pseudo cherry red spot may be seen when commotio involves the fovea. The fundus reflex may be notably white as opposed to red.
Optical coherence tomography (OCT) signs include increased reflectivity and thickness of the ellipsoid zone (EZ) with disruption of the interdigitation zone (IZ) and occasionally inner retinal layers.[4]
Optical Coherence Tomography Angiography (OCTA) may or may not show any significant microvascular changes in the superficial or deep capillary plexuses.[12][13] Montorio et al reported OCTA findings of 18 patients with Berlin's edema after blunt trauma over 6 months; an initial early decrease in vessel density was seen in superficial and deep capillary plexuses and in the radial peripapillary capillary plexus at 1 month, with gradual normalizing of the values at 6 months.[13]
Symptoms
Common symptoms include blurry vision, vision loss, or visual field defect immediately following trauma.
Diagnostic Procedures
- Dilated fundus examination
- OCT
- Fundus photography
- Ultrasonography (in cases with unclear media due to vitreous hemorrhage or anterior segment injury)
Differential Diagnosis
- Retinal ischemia
- Choroidal rupture
- Purtscher retinopathy
- Traumatic macular hole
- Chorioretinitis sclopetaria
- Retinal detachment
Management
Patients suffering substantial ocular trauma with commotio retinae should be followed with serial eye exams to evaluate for any additional treatable conditions. As commotio of the macula resolves, partial- or full-thickness macular holes can develop.
General Treatment
There is no approved or commonly used medical treatment for commotio retinae. However, in cases that do not resolve spontaneously, high-dose IV steroids have been anecdotally shown to reduce retinal swelling and improve visual acuity. [14]
Complications
Acute commotio retinae is commonly associated with traumatic macular hole, retinal tears, choroidal rupture, lens subluxation, hyphema, orbital fractures, late glaucoma, late cataract, late retinal tears, and widespread chorioretinal atrophy.[4][15]
Prognosis
While most patients recover completely, some patients will remain impaired with reduced vision or paracentral scotoma depending on the location of the injury.
Ahn et al created a 4-step grading system for prognosis by evaluating damage in photoreceptor layers. This classification is based on OCT findings, with increasing grades of pathology predicting poorer visual recovery:[4]
- Grade 1: increased reflectivity of the EZ with loss of ordinary definition of the photoreceptor lines
- Grade 2: loss of reflection in cone outer segment tips (IZ)
- Grade 3: loss of reflection in IZ and EZ
- Grade 4: loss of reflection in the IZ, EZ and external limiting membrane
Most cases of commotio retinae resolve within 4 weeks of injury, although some improvement can continue for up to 6 months.[2] However, some patients can have permanent macular damage with absolute or relative scotoma.[16] Patients with commotio retinae involving the macula have a poorer prognosis due to damage to the fovea along with increased risk of lamellar hole, macular hole, or permanent RPE atrophy as a secondary complication.[15] Studies have shown that 26% of patients with commotio retinae with macular involvement end up with permanent visual impairment (VA of <20/30).[2] In contrast, only 3% of patients with extramacular injury have permanent visual consequences. There are no treatments to improve outcomes in these patients.[2]
Additional Resources
- NIOSH. National Institute for Occupational Safety and Health. Eye Safety Injury and Illness Data. https://www.cdc.gov/niosh/topics/eye/injuryillness.html Accessed March 22, 2023.
References
- ↑ Berlin R. Sogenannten commotio retinae. So-called commotio retinae. Klin Monatsbl Augenheilkd 1873;1:42–78.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 BLANCH, R.J., UNDERSTANDING AND PREVENTING VISUAL LOSS IN COMMOTIO RETINAE, in College of Medical and Dental Sciences. 2014, University of Birmingham: Birmingham, UK. p. 581.
- ↑ 3.0 3.1 3.2 Hart, J.C. and R. Blight, Commotio retinae. Arch Ophthalmol, 1979. 97(9): p. 1738.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Ahn, S.J., et al., Optical coherence tomography morphologic grading of macular commotio retinae and its association with anatomic and visual outcomes. Am J Ophthalmol, 2013. 156(5): p. 994-1001.e1.
- ↑ Burke, M. , Lieu, P. , Abrams, G. & Boss, J. (2021). MACULAR CHOROIDAL THICKNESS IN UNILATERAL COMMOTIO RETINAE. Retinal Cases & Brief Reports, 15 (4), 417-420.
- ↑ 6.0 6.1 6.2 Mansour, A.M., W.R. Green, and C. Hogge, Histopathology of commotio retinae. Retina, 1992. 12(1): p. 24-8.
- ↑ Blanch, R.J., et al., Animal models of retinal injury. Invest Ophthalmol Vis Sci, 2012. 53(6): p. 2913-20.
- ↑ 8.0 8.1 Mansour AM and Shields CL. Microvascular Capillary Plexus Findings of Commotio Retinae on Optical Coherence Tomography Angiography. Case Rep Ophthalmol 2018; 9:473-478.
- ↑ Hashimoto R, Hirota A and Maeno T. Choroidal blood flow impairment demonstrated using laser speckle flowgraphy in a case of commotio retinae. Am J Ophthalmol Case Rep 2016; 4:30-34.
- ↑ JB, J., An ongoing tragedy: pediatric sports-related eye injuries. Semin Ophthalmol, 1990. 5: p. 216-223.
- ↑ Venkatesh R, Pereira A, Sangai S, Yadav NK. Hyporeflective micro-elevations and irregularity of the ellipsoid layer: novel optical coherence tomography features in commotio retinae. Can J Ophthalmol. 2020 Dec;55(6):492-499. doi: 10.1016/j.jcjo.2020.06.020. Epub 2020 Aug 24. PMID: 32853587.
- ↑ Mansour AM, Shields CL. Microvascular Capillary Plexus Findings of Commotio Retinae on Optical Coherence Tomography Angiography. Case Rep Ophthalmol. 2018 Nov 27;9(3):473-478. doi: 10.1159/000494916. PMID: 30631274; PMCID: PMC6323412.
- ↑ 13.0 13.1 Montorio D, D'Andrea L, Cennamo G. Retinal Vascular Features in Ocular Blunt Trauma by Optical Coherence Tomography Angiography. J Clin Med. 2020 Oct 16;9(10):3329. doi: 10.3390/jcm9103329. PMID: 33081316; PMCID: PMC7602990.
- ↑ Mendes S, Campos A, Beselga D, Campos J, Neves A. Traumatic Maculopathy 6 Months after Injury: A Clinical Case Report. Case Reports in Ophthalmology. 2014;5(1):78-82. doi:10.1159/000360692.
- ↑ 15.0 15.1 David Browning, M.P. What You Should Know About Blunt Trauma to the Eye: Commotio Retinae, Hyphema, Lens Dislocation, Vitreous Hemorrhage, Retinal Breaks, and Early and Late Glaucoma. [cited 2016 May 30th, 2016]; Available from: http://www.retinareference.com/diseases/9c563c5794aacd24/documents/9c563c5794/document.pdf.
- ↑ EM, E., Ocular damage after blunt trauma to the eye. Its relationship to the nature of the injury. Br J Ophthalmol, 1974. 58: p. 126-140.