Paracentral Acute Middle Maculopathy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Paracentral acute middle maculopathy (PAMM) is an optical coherence tomography finding seen in patients with retinal capillary ischemia and unspecific persistent scotomas. PAMM occurs as an isolated phenomenon or as a complicating feature of an underlying retinal vasculopathy or systemic disease.
Disease Entity
Paracentral acute middle maculopathy.
Disease
Paracentral acute middle maculopathy (PAMM) is a spectral-domain optical coherence tomographic (SD-OCT) finding first reported in 2013 by Sarraf and colleagues and interpreted as a possible more superficial variant of acute macular neuroretinopathy (AMN).
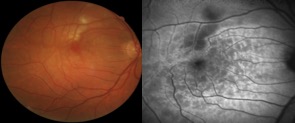
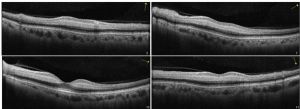
It is characterized by hyperreflective band-like, multiple, or isolated focal or diffuse lesions visible at the level of the inner nuclear layer (INL) in patients presenting with acute onset of negative scotoma. It is descriptively termed PAMM due to parafoveal position of the causative grey lesions with near-infrared reflectance imaging, and the SD-OCT localization of involvement to the middle layer (INL) of the retina.
Etiology
The etiology is unknown. A vascular etiology is hypothesized.
Risk Factors
Environmental risk factors have been proposed for PAMM, such as vasopressor exposure (eg, caffeine, vasopressors, oral contraceptives) , and PAMM has recently been associated with numerous retinal vascular diseases including diabetic retinopathy, hypertensive retinopathy, sickle cell retinopathy, Purtscher retinopathy, central retinal vein occlusion, and retinal artery occlusion. A single case of PAMM in an uncomplicated pregnancy has been described.
Pathophysiology
PAMM is an SD-OCT abnormality that may herald the presence of a secondary underlying condition predisposing to microvascular ischemic injury. Localized retinal capillary ischemia at the level of intermediate plexus is proposed as the mechanism underlying the development of these lesions.
Primary Prevention
None.
Diagnosis
Clinical diagnosis is based on a patient’s history of acute onset negative scotoma with no other visual or ocular symptoms. Funduscopic examination may not reveal significant abnormalities. PAMM lesions appear as subtle, whitish parafoveal lesions deeper within the retina, smoother in contour and greyer than cotton-wool spots. Emboli may be present at the base of a focal PAMM lesion or along retinal arterial branches, and they may be visible on high-magnification fundoscopy. As the clinical appearance can be quite subtle by funduscopic examination, reliance on supplemental diagnostic imaging techniques is critical. To date, near-infrared reflectance, fundus autofluorescence and SD-OCT imaging remain the most sensitive modalities. En-face OCT and OCT-angiography have recently emerged as promising tools in the diagnosis and management of these patients.
History
In patients with PAMM, the average age of onset is the late 50s to the 60s, particularly when PAMM is a complicating feature of an underlying retinal vasculopathy or systemic disease (see Risk Factors, above). However, it may also be idiopathic and may develop in younger and otherwise healthy individuals whose systemic history is normal. Patients report the sudden onset of paracentral scotomas without other ocular or visual symptoms.
Physical Examination
Extraocular physical examination has no distinct features. For ocular features, see Signs, below.
Signs
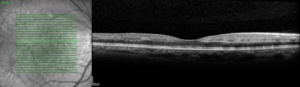
On OCT, the acute lesions of PAMM characteristically appear as placoid, hyperreflective bands at the level of the INL, sparing the outer retina, showing corresponding hypoautofluorescence on fundus autofluorescence and are hyporeflective and well-demarcated on near infrared reflectance. A legacy of thinning and atrophy of the affected INL ensues. It is responsible for the permanent visual deficits that patients with PAMM typically experience.
Optical coherence tomography angiography (OCTA) produces detailed, high-resolution images of the retinal vasculature segmented by layer. Recent cases of PAMM have been imaged using simultaneous en face OCT and OCTA. En face OCT may emerge as the preferred method to image and follow the clinical course of these patients. Focal vascular remodeling with pruning of the intermediate and posterior capillary plexus over time seems to coincide with evolution of the SD-OCT lesions from hyperreflective plaques into INL atrophy.
Differential diagnosis
The main differential diagnosis is acute macular neuroretinopathy (AMN).
Acute macular neuroretinopathy is a much rarer entity (less than 100 reported cases in English literature in the last 40 years) than PAMM, and it typically affects healthy women who are in their teens to their 30s. The hyperreflective band-like AMN lesions develop slightly lower at the junction of the outer plexiform and outer nuclear layers. There may be associated persistent disruption of the ellipsoid and interdigitation zones that may help to explain the long-standing symptomatic scotomas in some patients with AMN, compared with patients with PAMM.
Management
PAMM may be idiopathic and may even develop in young and healthy individuals with an otherwise normal ocular examination result. However, for a patient with PAMM who has an apparently healthy fundus, an appropriate systemic work-up to exclude contributing systemic or cardiovascular risk factors, such as arterial hypertension, dyslipidemia, or diabetes, is advisable. Diffuse lesions can harbor an occult central retinal artery occlusion and, in such instances, it is mandatory to rule out underlying carotid disease (carotid ultrasound imaging) or giant cell arteritis (ESR, RCP). Wide field fluorescein angiography may also help to rule out associated retinal artery occlusion.
General treatment
None.
Medical therapy
No specific medical intervention can be performed, and underlying vascular or systemic disease, if present, must be addressed accordingly.
Medical follow-up
Follow-up is at the discretion and comfort level of the physician. It may be every few weeks or months, simply to document the course of the disease.
Surgery
Carotid endarterectomy may be necessary if significant carotid obstruction is present.
Complications
None.
Prognosis
Full resolution of scotomas has been reported, but partial resolution is the most common outcome. Significant visual impairment is uncommon.
References
- Rahimy E, Kuehlewein L, Sadda SR, Sarraf D. Paracentral Acute Middle Maculopathy: What We Knew Then and What We Know Now. Retina. 2015 Oct;35(10):1921-30. doi: 10.1097/IAE.0000000000000785. PMID: 26360227.
- Chen X, Rahimy E, Sergott RC, Nunes RP, Souza EC, Choudhry N, Cutler NE, Houston SK, Munk MR, Fawzi AA, Mehta S, Hubschman JP, Ho AC, Sarraf D. Spectrum of Retinal Vascular Diseases Associated With Paracentral Acute Middle Maculopathy. Am J Ophthalmol. 2015 Jul;160(1):26-34.e1. doi: 10.1016/j.ajo.2015.04.004. Epub 2015 Apr 4. PMID: 25849522.
- Yu S, Pang CE, Gong Y, Freund KB, Yannuzzi LA, Rahimy E, Lujan BJ, Tabandeh H, Cooney MJ, Sarraf D. The spectrum of superficial and deep capillary ischemia in retinal artery occlusion. Am J Ophthalmol. 2015 Jan;159(1):53-63.e1-2. doi: 10.1016/j.ajo.2014.09.027. Epub 2014 Sep 22. PMID: 25244976.
- Rahimy E, Sarraf D, Dollin ML, Pitcher JD, Ho AC. Paracentral acute middle maculopathy in nonischemic central retinal vein occlusion. Am J Ophthalmol. 2014 Aug;158(2):372-380.e1. doi: 10.1016/j.ajo.2014.04.024. Epub 2014 May 1. PMID: 24794089.
- Munk MR, Jampol LM, Cunha Souza E, de Andrade GC, Esmaili DD, Sarraf D, Fawzi AA. New associations of classic acute macular neuroretinopathy. Br J Ophthalmol. 2016 Mar;100(3):389-94. doi: 10.1136/bjophthalmol-2015-306845. Epub 2015 Aug 20. PMID: 26294104.