Pachychoroid Spectrum
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Pachychoroid Spectrum refers to a group of clinical entities with a common characteristic: a pachychoroid. This term derives from the Greek word παχύ, pachy, thick. It refers to an anatomic choroidal characteristic with a thickened choroid. Typically, pachychoroid is studied and visualized with Enhanced Depth Imaging optical coherence tomography (EDI-OCT) or Swept Source OCT (SS-OCT).
Anatomy of choroid
- The choroid is responsible for vascular support to the external part of the retina, and its functional and structural integrity is essential for normal retinal function. A compromised volume or flow in its circulation could result in dysfunction and death of photoreceptor and retinal pigment epithelium (RPE). The choroidal blood supply derives from branches of the anterior and posterior ciliary arteries. The choriocapillaris has large diameter capillaries (20-25 μm) and fenestrations of 700-800 nm diameter, allowing more rapid transport of bigger molecules.
Histologically, the choroid is composed of 5 layers, which are in order from inner (retinal side) to outer (scleral side):
- Bruch Membrane
- Ruysch Layer (Choriocapillaris)
- Sattler's Layer (Layer of medium diameter blood vessels)
- Haller´s Layer (Layer of large diameter blood vessels)
- Suprachoroidea (Transitional zone between choroid and sclera)
Anatomy of choroid on OCT
Through the use of EDI–OCT and SS-OCT, some important anatomical characteristics can be defined. The choroid is thickest in the subfoveal region, thinner in the nasal region, and has a progressive thinning through the temporal region. Subfoveal choroidal thickness (SFCT) is approximately 300 microns, and the median choroidal thickness is approximately 260 microns. However, choroidal thickness varies based on age, gender, ethnicity, and other factors, including the measuring instrument. There is an age-related choroidal thickness reduction of about 10-15 microns per decade of life. Examining the choroidal layers, the submacular central thickness in Sattler's layer is approximately 87 +/- 56 microns, and Haller's layer is approximately 141 +/- 50 microns.
Disease Entity
Disease
The Pachychoroid Spectrum refers to a group of clinical entities with a common characteristic of a thickened choroid. These share the same underlying pathological mechanism. These entities are pachychoroid pigment epitheliopathy, central serous chorioretinopathy (CSCR), pachychoroid neovasculopathy and polypoidal choroidal vasculopathy. There have been some other entities described that are associated with a thick choroid, including Vogt-Koyanagi-Harada disease (VKHD).
Etiology
Its common characteristics are a thick choroid with dilated and hyperpermeable vessels, which may cause focal Bruch's membrane and RPE disruption that could lead to serous retinal detachment.
Risk Factors
Common risk factors include: "Type A" personality, emotional stress, pregnancy, tobacco use, corticosteroids, and other sympathomimetics. Certain herbal supplements may also have glycogenic properties associated with pachychoroid development.
Specific Pathologies
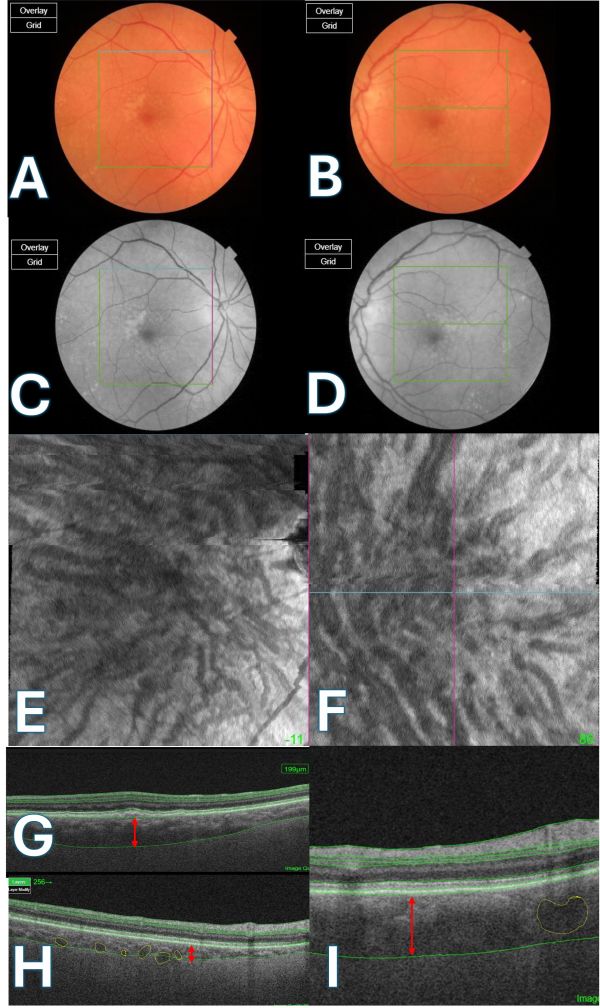
Pachychoroid Pigment Epitheliopathy (PPE)
Clinical Findings
This is usually a silent Disease. visual acuity is normal. The fundus appears orange-reddish with the absence of fundus tessellation. RPE lesions that could cause drusenoid fundus without subretinal fluid. PPE is also called forme fruste central serous chorioretinopathy.
Ancillary Testing
OCT:
- Thick choroid and large choroidal vessels beneath elevations on RPE and
- sub-RPE drusen like deposits.
ICGA (Indocyanine Green Angiography):
- Choroidal hyperpermeability and hyperpermeability co-existent with areas of RPE change.
FAF (Fundus Autofluorescence):
- Granular and mixed stippled hyper-hypoautofluorescence.
Central Serous Chorioretinopathy (CSCR)
Clinical Findings
It commonly presents at age 20-50, with a gender predilection of male: female 6:1, has an incidence of about 5-6/100,000, best corrected visual acuity 20/20 – 20/200 with a median 20/30. Characteristic presenting symptoms include metamorphopsia, blurred vision, micropsia, and relative scotoma. Findings typically resolve within six months. When findings persist for longer, these may be classified as chronic CSCR.
Physical Examination
Usually, a round or oval area of subretinal fluid may involve the fovea. Multifocal CSCR with multiple areas of subretinal fluid may also be seen.[1] CSCR may present as a bullous, inferior, non-rhegmatogenous peripheral retinal detachment, especially in patients receiving systemic steroids. Other features include an absent foveal reflex, yellow-gray elevation, and speckled or grouped RPE (this finding may suggest chronicity).
Ancillary Testing
OCT:
- Pachychoroid + serous RPE detachment + subretinal fluid.
- Serous PED points towards the diagnosis of CSCR.
- There may be outer retinal sagging.
- The RPE in areas without serous PED is usually straight in contrast to inflammatory pathologies, including VKHD and choroidal granuloma
ICGA:
- Choroidal congestion and
- hyperpermeability with multifocal hypofluorescent areas.
Fluorescein angiography (FA):
- Serous RPE detachment with leak/s at the level of the retinal pigment epithelium.
- The patterns of leaks include
- inkblot leak
- smokestack leak
- diffuse leaks
FAF:
- Speckled Hyperautofluorescence and eventually gravitational zones (RPE tracks).
Risk Factors
- Type A personality,
- emotional stress,
- systemic hypertension,
- gastroesophageal reflux disease,
- pregnancy,
- organ transplantation,
- systemic lupus erythematosus,
- tobacco,
- alcohol,
- membranoproliferative glomerulonephritis type II,
- Helicobacter pylori infection,
- autoimmune disorders,
- Medications: corticosteroids, psychopharmacologic medications, MDMA, antacids and anti-reflux medications, over-the-counter sympathomimetics, antibiotics, antihistamines, sildenafil citrate.
Differential Diagnosis
Differential diagnoses include choroidal neovascular membrane specifically occult ones, optic disc pit, polypoidal choroidal vasculopathy, choroidal melanoma, choroidal metastasis, peripheral retinal break, choroidal hemangioma, uveitis, Harada disease, optic neuritis, papilledema, vitreal traction, macular hole, systemic hypertension.
Treatment
The initial treatment of choice is observation; in most cases, it resolves spontaneously. If it fails to improve in 3-6 months, it should be considered for treatment with laser photocoagulation (if the leakage zone is > 200 microns of the foveal region) or photodynamic therapy. Indications for early treatment include professional requirements, the patient's desire for early visual recovery, one-eyed status, recurrent disease, and poor vision in the fellow eye due to chronic CSCR. However, there may be a trend for early treatment of CSCR as delay in spontaneous resolution of subretinal fluid may lead to irreversible functional damage.[2][3]
Prognosis
Almost always, the patient will have a visual acuity of 20/40 or above, but metamorphosis may persist .
Pachychoroid Neovasculopathy/ Polypoidal Choroidal Vasculopathy (PCV)
Clinical Findings
Clinical findings include blurred vision. There may be reduced fundus tessellation with or without serous retinal detachment.
Ancillary Testing
OCT:
- Pachychoroid with neovascularization type 1 (sub-RPE),
- large choroidal vessels obliterating choriocapillaris and Sattler's layer,
- large choroidal vessels obliterating choriocapillaris and Sattler's layer,
- Choroidal vessels between Bruch membrane and RPE, also the “double layer sign”.
- These changes could progress to polypoidal vascular lesions (Polypoidal Choroidal vasculopathy),
- Pigment epithelial detachments may have thumb shape, M shape, or notch,
- There is a prominence of subretinal fluid compared to intraretinal fluid.
ICGA:
- Choroidal hyperpermeability with hyperfluorescent early dots and vascular network with dilated choroidal vessels. These vessels could progress to polypoidal vasculopathy.
Treatment
In cases of chronic CSCR and PCV, anti-VEGF (anti-vascular endothelial growth factor) agents and/or photodynamic therapy may be considered.
References
- ↑ Gupta A, Tripathy K. Central Serous Chorioretinopathy. In: StatPearls. Treasure Island (FL): StatPearls Publishing; February 22, 2023.
- ↑ Tripathy K, Mishra C, Addya S. Commentary: Available evidence on early treatment of central serous chorioretinopathy. Indian J Ophthalmol. 2021;69(9):2348-2349. doi:10.4103/ijo.IJO_809_21
- ↑ Goel N, Mehta A, Gupta AK. Multifocal electroretinography-assisted anatomical and functional evaluation of subthreshold green laser in acute central serous chorioretinopathy. Indian J Ophthalmol. 2021;69(9):2341-2346. doi:10.4103/ijo.IJO_3401_20
Further reading
1. Warrow DJ, Hoang Q V., Freund KB. Pachychoroid Pigment Epitheliopathy. Retina. 2013;33(8):1659-1672. doi:10.1097/IAE.0b013e3182953df4.
2. Vuong VS, Moisseiev E, Cunefare D, Farsiu S, Moshiri A, Yiu G. Repeatability of Choroidal Thickness Measurements on Enhanced Depth Imaging Optical Coherence Tomography Using Different Posterior Boundaries. Am J Ophthalmol. 2016;169:104-112. doi:10.1016/j.ajo.2016.06.023.
3. Pulido JS, Kitzmann AS, Wirostko WJ. 6.30 - Central Serous Chorioretinopathy. Fourth Edition. Elsevier Ltd; 2016. doi:10.1016/B978-1-4557-3984-4.00171-8.
4. Pang CE, Shah VP, Sarraf D, Freund KB. Ultra-widefield imaging with autofluorescence and indocyanine green angiography in central serous chorioretinopathy. Am J Ophthalmol. 2014;158(2):362-371.e2. doi:10.1016/j.ajo.2014.04.021.
5. Pang CE, Freund KB. Pachychoroid neovasculopathy. Retina. 2015;35(1):1-9. doi:10.1097/IAE.0000000000000331.
6. Miyake M, Ooto S, Yamashiro K, et al. Pachychoroid neovasculopathy and age-related macular degeneration. Sci Rep. 2015;5:16204. doi:10.1038/srep16204.
7. Mikhail M, Nofal N. WITH PERIPHERAL TEAR OF THE RETINAL PIGMENT EPITHELIUM IN. :1-4.
8. Maruko I, Iida T, Sugano Y, et al. Subfoveal choroidal thickness after treatment of Vogt-Koyanagi-Harada disease. Retina. 2011;31(3):510-517. doi:10.1097/IAE.0b013e3181eef053.
9. Maruko I, Iida T, Sugano Y, Go S, Sekiryu T. Subfoveal Choroidal Thickness in Papillitis Type of Vogt-Koyanagi-Harada Disease and Idiopathic Optic Neuritis. Retina. 2016;36(5):992-999. doi:10.1097/IAE.0000000000000816.
10. Labriola LT, Legarreta AD, Legarreta JE, et al. Imaging With Multimodal Adaptive-Optics Optical Coherence Tomography in Multiple Evanescent White Dot Syndrome: the Structure and Functional Relationship. Retin Cases Brief Rep. 2016:1-8. doi:10.1097/ICB.0000000000000271.
11. Kuroda Y, Ooto S, Yamashiro K, et al. Increased Choroidal Vascularity in Central Serous Chorioretinopathy Quantified Using Swept-Source Optical Coherence Tomography. Am J Ophthalmol. 2016;169:199-207. doi:10.1016/j.ajo.2016.06.043.
12. Ghadiali Q, Dansingani KK, Freund KB. Focal Choroidal Excavation and Choroidal Neovascularization With Associated Pachychoroid. Retin Cases Brief Rep. 2016;i:1. doi:10.1097/ICB.0000000000000301.
13. Gallego-Pinazo R, Dolz-Marco R, Gómez-Ulla F, Mrejen S, Freund KB. Pachychoroid diseases of the macula. Med hypothesis, Discov Innov Ophthalmol. 2014;3(4):111-115. http://www.ncbi.nlm.nih.gov/pubmed/25756060%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4352204.
14. Esmaeelpour M, Kajic V, Zabihian B, et al. Choroidal Haller’s and Sattler’s layer thickness measurement using 3-dimensional 1060-nm optical coherence tomography. PLoS One. 2014;9(6). doi:10.1371/journal.pone.0099690.
15. Dolz-marco BYR, Dansingani KK, Freund B. COVER FOCUS THE PACHYCHOROID CLINICAL SPECTRUM. 2016;(June):57-60.
16. Dansingani KK, Naysan J. En Face Imaging of Pachychoroid Swept-Source Optical Coherence. 1:1-18. doi:10.1097/IAE.0000000000000742.
17. Dansingani KK, Balaratnasingam C, Klufas MA, Sarraf D, Freund KB. Optical Coherence Tomography Angiography of Shallow Irregular Pigment Epithelial Detachments In Pachychoroid Spectrum Disease. Am J Ophthalmol. 2015;160(6):1243-1254. doi:10.1016/j.ajo.2015.08.028.
18. Chorioretinopathy CS, Detachments E. C h a p t e r 1 0 Central Serous Chorioretinopathy and Other Exudative Detachments. 2017. doi:10.1016/B978-0-323-28792-0.00010-7.
19. Chhablani J, Wong IY, Kozak I. Choroidal imaging: A review. Saudi J Ophthalmol. 2014;28(2):123-128. doi:10.1016/j.sjopt.2014.03.004.

